
We can “print” new body parts.
Imagine being able to manufacture knee cartilage, heart valves, muscle tissue, and skin at the touch of a button. That’s the aim of bioprinting, a technique that creates human tissue using a special “ink” made from donor stem cells. “These printers use stem cells and special gels to build living, 3-D structures one layer at a time,” says Jordan Miller, PhD, a postdoctoral fellow at the University of Pennsylvania.
Right now, bioprinting is producing only thin sheets of tissue, but scientists hope that soon the manufactured parts will help strengthen skin, bones, muscles, cartilage, and even kidneys and bladders. The long-term goal: “If you needed a transplant, you wouldn’t have to wait for a donor or use immunosuppressant drugs,” Miller says. “We’d make a replacement organ from your own cells.”
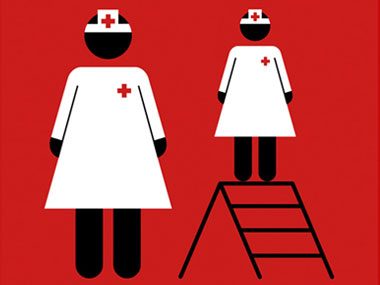
CPR just got easier for rescuers of all sizes.
Sometimes the most dramatic lifesaving gains come from the lowest-tech tools. Dana Edelson, MD, assistant professor at the University of Chicago, found it difficult to do CPR chest compressions deeply enough to effectively restart her patients’ hearts. “I’m five foot one and can’t generate the 60 kilos [about 130 pounds] of force you need standing at a hospital bed,” she says. Her solution: Equip all her hospital’s units with simple step stools so that shorter (under five foot six) clinical workers could apply more body weight to the task.
After making the change, she proved its success. Her study found that standing on a stool helped rescuers deepen their compression on training dummies by an extra centimeter—“a big boost,” Edelson says, since she’d previously shown that just a half-centimeter increase doubled the odds that a cardiac-arrest patient’s heart could be coaxed back to beating. “The reality,” says Edelson, “is that rescuers aren’t all the same any more than patients are.”

We can treat Alzheimer’s before it’s obvious.
The key to improving the brain function of people with Alzheimer’s disease may not be more-effective drugs but how those drugs are used. Since Alzheimer’s is difficult to detect early, drug treatment generally begins after brain damage has already occurred. Now three large trials are testing potential Alzheimer’s drugs in a new way: treating people who are at a high risk of developing Alzheimer’s years before their symptoms become obvious. In one study, the drug solanezumab became the first to demonstrate it could actually slow the progression of the disease. The effect was small but might be much more significant if the drug is given earlier.
“This is really important,” says Bruce Sigsbee, MD, president of the American Academy of Neurology. “The challenge will be to recognize the disease early enough to apply the drug.” Fortunately, scientists are working on just that, and they have started to identify, decades before symptoms occur, changes in the brains of people in their 20s who are destined to develop the inherited form of the disease.

Tweets are helping uncover public heath trends.
Researchers are now using social media to both track disease and predict your chances of getting sick. When a deadly cholera epidemic broke out in Haiti in 2010, informal chatter about it on social-media sites such as Twitter rose and fell with the number of official cases. The information gleaned from tweets beat the official data in the country by about two weeks.
Now researchers are using this new tool to inform the public. In one study, researchers used GPS-tagged tweets from more than 600,000 New Yorkers over a month to show where flu was spreading in the city, with hot spots visible on a map in real time. Another possible use: preventing food-borne illness. “If you’re interested in a restaurant where the data show that 20 percent of customers get sick the day after eating there, you might make another choice,” says University of Rochester postdoctoral fellow Adam Sadilek, PhD.

Safer surgery means no tool left behind.
Every once in a while—estimates range from once in 1,000 to once in 18,000 operations—surgeons leave an item, often a surgical sponge, inside a patient’s body, increasing the risk of infection and even death. “It doesn’t happen frequently,” says Hong Jin Kim, MD, associate professor of surgery at the University of North Carolina School of Medicine, “but these should be ‘never events.’ ” Even though rigorous protocols are in place to prevent these lapses, most rely on simple counting, which means human error is always possible.
Now a new “magic wand” that uses radiofrequency technology can help prevent such terrible mistakes. Sponges and pads are tagged with a signal-emitting device about the size of a rice kernel. Waving the wand over the body before sewing up an incision picks up any signals from the surgical site and alerts doctors to tagged items that were overlooked. A study documented 35 miscounts in 2,285 patients—and one instance of a sponge almost being left behind—with traditional methods. The number of surgical items left behind using the radiofrequency system: zero.

A “super vaccine” recognizes cancerous cells.
Cancer treatments that help the body heal itself are a hot research topic since they may help people avoid surgery, radiation, and chemotherapy. One especially promising approach is a vaccine that trains the immune system to recognize a trait unique to cancerous cells: a protein (called MUC1) that develops a distinctive sugar pattern on its surface when cells turn malignant. Once the vaccine prompts the immune system to recognize those sugars as a threat, the body’s natural defenses can destroy the cancerous cells without harming healthy tissue. According to the Mayo Clinic and University of Georgia (which are collaborating on the vaccine), MUC1 can be found on more than 70 percent of deadly cancers, including breast, lung, pancreatic, and some colon tumors.
Another use: When it’s given after conventional treatments like radiation and chemotherapy, “we envision the vaccine will clear all remaining tumor cells so the cancer won’t come back,” says Geert-Jan Boons, PhD, associate director of the University of Georgia’s Complex Carbohydrate Research Center. Human trials are now under way.

Facebook saves lives by generating organ donor “likes.”
Last spring, Facebook added a feature that allowed users to share their organ donor status. Within six months, over 400,000 Facebook users declared themselves donors, kicking off an awareness campaign that increased the number of registered donors nationwide. That’s good news for the nearly 7,000 people in the United States who would otherwise die each year waiting for an organ transplant. Facebook even provides a link to states’ online donor registries for people who want to sign up.
Says David Fleming, president and chief executive officer of Donate Life America, which partnered with the social-media giant, “One simple change to Facebook has raised awareness of organ, eye, and tissue donation in a major way.” And that’s a great big Like.
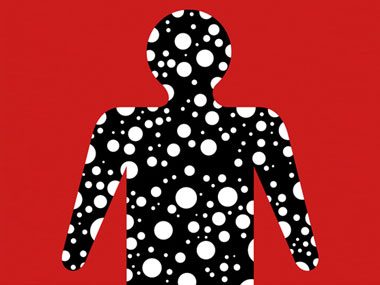
New genetic maps of the body’s bacteria help fight disease.
Scientists from 80 universities and research institutions have spent the past five years genetically mapping 81 to 99 percent of our normal bacterial makeup, our “microbiome”—trillions of microorganisms that live inside each of us. Most of these “bugs” are good, or at least not harmful. Sorting out what they are, why they live within us, and what’s normal will help us understand disease, according to Rob Knight, PhD, associate professor at the BioFrontiers Institute at the University of Colorado Boulder.
The Human Microbiome Project has already turned up a few surprises. “Lean and obese people have markedly different communities in the gut,” Knight says. “We don’t know if microbes contribute to weight gain or if they change when people become obese.” Further research will explore how bacteria affect a wide variety of conditions, including allergies, Crohn’s disease, esophageal cancer, and psoriasis. “It’s a very exciting time,” says Knight.

Scientists develop an easier colon cancer test.
An experimental new test may soon replace the dreaded colonoscopy as a way of screening for colon cancer and its precursors. The test searches for two DNA cancer flags along with traces of blood in a stool sample. Together, these three markers identified 98 percent of cancers and 57 to 83 percent of cancer precursors in a preliminary study presented to the American Association for Cancer Research. The company behind the test plans to apply for FDA approval soon.
“The test detects even small signs of disease at very early stages—and early diagnosis is the key to good outcomes,” says Cory Abate-Shen, PhD, associate director of Columbia University’s Herbert Irving Comprehensive Cancer Center in New York.

Doctors vow to practice what they preach.
A new Patient Promise campaign has so far gathered 673 signatures from doctors at 57 medical institutions around the country. What are these doctors promising? They’re vowing to become healthy role models for their patients by agreeing to statements like the following: “I will consume a balanced and nutritious diet,” “I will engage in regular physical activity,” “I will diminish personal stressors and look after my mental well-being.”
Research shows that physicians who eat poorly or don’t exercise may be less likely to encourage healthy habits in their patients. “Yet five or six of every ten clinicians are overweight or obese,” says Shiv Gaglani, a second-year student at Johns Hopkins University School of Medicine. That’s why Gaglani and his roommate David Gatz began the Patient Promise campaign. Gaglani says the majority of signers are students, but some of the first adopters are already working at hospitals. “We’re training a new generation to lead by example.”