What Are Heart Arrhythmias? Symptoms, Risk, and Treatments for Irregular Heartbeats
Updated: Apr. 13, 2021
If your heart beats too fast, too slowly, or has an irregular rhythm, you may have an arrhythmia.
What is arrhythmia?
You can go months without even noticing your heartbeat. As long as it’s pumping along as it should, your heart can be easy to ignore. But occasionally, you might notice something odd—an irregular heartbeat, which is also called a heart arrhythmia. Your heart might beat a little faster, slower, or feel somehow off.
“The term arrhythmia refers to what is essentially a short circuit in the electrical system of the heart cells that coordinate contraction of the heart and the rate at which the heart beats,” says Hugh Parker, MD, a cardiologist with UCHealth Heart and Vascular Center–Cherry Creek and assistant professor with the CU School of Medicine, Denver. It might feel like your heart is “fluttering” or skipping a beat. Or possibly it might feel like your heartbeat is very fast and pounding.
Many arrhythmias are benign, but they may signal a serious or life-threatening condition. Here’s what you should know about the risks and how to protect your heart. (Be sure to know the signs of an unhealthy heart.)
How a heart arrhythmia is created
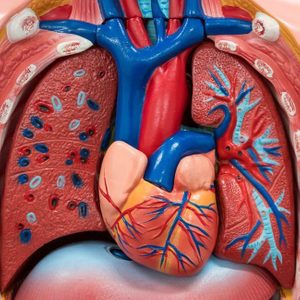
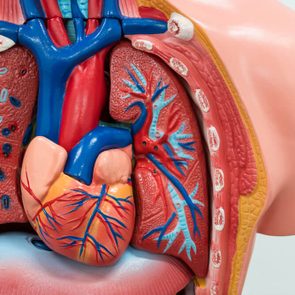
In a healthy heart, separate processes work seamlessly side-by-side to keep blood pumping through the body. But sometimes, one of these processes can slip. Here’s the breakdown of how the heart works and what happens to cause an arrhythmia.
“The heart has two systems that work together to ensure that the heart efficiently moves blood throughout the body. The first of these is the pumping function of the heart. The normal heart has four chambers that are separated by valves that ensure that the blood moves in one direction through the heart chambers and blood vessels,” says Lee Goldberg, MD, a cardiologist and section chief, advanced heart failure and cardiac transplant at the University of Pennsylvania in Philadelphia.
(These are the ways to keep your heart valves healthy.)
A second system comes into play to keep blood moving in the right direction through the network of arteries and veins.
“In order to coordinate the synchronized motion of each of the heart chambers, to allow maximum efficiency, and to control the heart rate, an electrical system is wired throughout the heart,” says Dr. Goldberg, who’s also a professor of cardiovascular medicine in the Perelman School of Medicine at the University of Pennsylvania.
When the “wiring” is out of whack in the electrical system, an arrhythmia ensues. Repeat heart arrhythmias that are unrecognized or left untreated can increase the risk of developing heart failure.

Types of heart arrhythmias you should know
There are many different cardiac arrhythmias, and the type and severity will influence how your doctor treats the problem.
“We typically worry about heart arrhythmias when they last long enough to cause concerning symptoms—such as dizziness, lightheadedness, loss of consciousness, or in the extreme case, death. Or when they are associated with an increased risk of another serious health event,” says Ameya Kulkarni, MD, an interventional cardiologist at Kaiser Permanente in Tysons, Virginia, and chair of the Mid-Atlantic Kaiser Permanente Cardiovascular Institute.
“For example, the irregular heartbeat condition called atrial fibrillation (or AFib) can increase your risk of stroke,” he explains.
Atrial fibrillation
AFib causes an irregular and often rapid heartbeat (up to 400 beats per minute) in the upper chambers of the heart. The atria quivers (fibrillate) instead of beating normally, making the bottom chambers (the ventricles) beat irregularly and chaotically. Some people might not even feel the chaos happening in their chest, while others feel palpitations and other symptoms.
“Among rhythms that last more than a few beats, atrial fibrillation is the most common rhythm,” says Dr. Kulkarni. At least 2.7 million Americans are living with AFib, according to the American Heart Association. And it’s very common among the elderly.
“As we get older the top chamber of our heart stretches, and AFib is likely a reflection of this process. AFib affects about 9 percent of people 65 and older,” says Dr. Kulkarni. Having this condition increases your risk for stroke, heart failure, and other heart problems.
Atrial flutter
An atrial flutter (AFL) is caused by a single abnormal electrical circuit circulating in the atrium about 300 times per minute, causing the atria to beat quickly and flutter instead of fully squeezing. Even though AFL is fast like the AFib, the heart rhythm is regular, not chaotic like AFib. And AFL isn’t life-threatening like AFib. But left untreated, the side effects can cause wear and tear on the heart, making it harder for the heart to pump blood.
Ventricular tachycardia
Ventricular tachycardia is characterized by a rapid and abnormal heart rate of three or more consecutive heartbeats at more than 100 beats per minute. The heart rate is so fast that it doesn’t give the heart enough time to fill with blood before it contracts again, affecting the blood flow to the rest of the body.
If it only lasts a few seconds, it might not be anything to worry about. However, if it lasts longer and there is no pulse, a person must receive CPR or defibrillation immediately to restore a normal rhythm. If the normal rhythm isn’t restored within a few minutes, brain and heart damage occur and possibly death.
Ventricular tachycardia is usually triggered by another heart condition such as heart disease. But in some cases, it can be triggered by certain medications; occasionally there is no obvious cause.
(These are the heart failure stages to know.)
Ventricular fibrillation
Ventricular fibrillation, also known as VFib, happens when disorganized electrical signals tell the ventricles to quiver instead of pump, halting the blood flow to the rest of the body. In some people, VFib may occur several times a day. This is called an “electrical storm.”
However, when VFib leads to a drop in blood pressure and loss of consciousness, there’s no time to waste. It can lead to sudden cardiac arrest and death if the normal heart rhythm isn’t restored within a few minutes. According to the Heart Rhythm Society, sudden cardiac arrest caused by ventricular fibrillation is responsible for half of all heart-related deaths. CPR or defibrillation is needed to restore the rhythm.
(Learn more about ventricular arrhythmias.)
Heart arrhythmia symptoms
Whether a heartbeat is too fast, too slow, or chaotic, the effects on the body are similar. In addition to the irregular heartbeat you may or may not notice, here are some more common symptoms of heart arrhythmias:
- Tiredness and weakness
- Dizziness, lightheadedness
- Feeling faint
- Low blood pressure
- Anxiety
- Trouble breathing
- Blurred vision
- Confusion
- Sweating
- Chest pain
- Sudden loss of consciousness
Heart arrhythmia causes
The switches in the heart’s electrical system have connections to the nervous system. Here, there are sensors and receptors that can detect and respond to hormones and chemicals in the blood. That response could be an abnormal heart rate that speeds up, slows down, or chaotic. Heart rhythms can be caused or triggered by a host of things.
“Some arrhythmias can be triggered by activities of daily life, while many can occur independently. Potential triggers can include excessive caffeine, alcohol, infection, dehydration, stress, or even lack of rest,” says Rakesh Latchamsetty, MD, an assistant professor and electrophysiologist cardiologist (a cardiologist specializing in heart rhythm problems) at the Michigan Medicine Frankel Cardiovascular Center in Ann Arbor, Michigan.
The list of culprits is long. Here are some of the more common causes and triggers:
- High blood pressure
- Low blood sugar
- Dehydration
- Electrolyte imbalance
- Untreated sleep apnea
- Over-the-counter cold, allergy, cough, and dietary medicines or supplements
- Prescription medications
- Hormone fluctuations in menstruating and pre-menopausal women
- Strong emotions (anxiety, stress, surprise, anger)
- Very high altitude
- Untreated sleep apnea
- High-protein or liquid-based diet
- Heart failure
- Heart valve disease
- Heart surgery
- Pneumonia
- Lung cancer
- Thyroid disease
- Diabetes
Remember, triggers vary by individual. For example, one person may not be affected by a cup of coffee, but it may cause a flare-up for another. Track everything that triggers your arrhythmia and let your doctor know.
Diagnosing heart arrhythmias
When you’re experiencing lightheadedness, shortness of breath or passing out, and/or if palpitations don’t go away quickly and consistently last a long time (around 10 minutes), you should see your doctor immediately, Dr. Kulkarni says. Your doctor will also ask questions about your medical and family history, about your symptoms, and the type of activities you are doing. This information helps determine if there are any underlying conditions or complications. These can include sleep apnea, previous heart attack, or Covid-19.
Your doctor will listen to your heart for its rate, rhythm, and murmurs and check for swollen legs and feet, an indicator of an enlarged heart or heart failure. Next, blood tests and imaging tests may be ordered to determine the type and severity of the arrhythmia.
Here are some common tests:
Electrocardiogram: A noninvasive test that records the speed of the heartbeat and shows if the rhythm is regular or irregular
Echocardiogram: An ultrasound to see how the heartbeats how fast your heart is beating and whether the rhythm is regular or irregular
Holter or event monitors: Types of monitors worn for a day or two to record the heart’s electrical activity while doing your normal activities
Stress test: Usually done on a treadmill or stationary bike for people who experience irregular heartbeats or even chest pain while exercising. If an arrhythmia is triggered, the abnormal heartbeat is assessed.
Treating heart arrhythmias
The outcome of heart arrhythmia sways much like a pendulum. It’s either incidental and doesn’t require treatment, or it can cause sudden death.
“The treatment of an arrhythmia, when treatment is necessary, is entirely dependent on the type of arrhythmia present. Having an arrhythmia is kind of like saying, ‘There is a mammal in the house.’ If it’s a mouse, no worries. If it’s a rabid tiger, big problem,” says Dr. Parker.
“Treatments can include lifestyle modification, medications or what we call ablation procedures, which are procedures where a specialist uses various techniques, usually catheter-based, to burn away the cells inside the heart that are causing problems,” says Dr. Parker.
Medications to treat arrhythmias include:
Beta-blockers: They slow heart rate and block adrenaline, which can cause irregular heart rhythms.
Calcium channel blockers: These blockers slow the heart rate by keeping calcium from entering the cells of the heart.
Potassium channel blockers: They slow down the heart’s electrical impulses by blocking potassium from entering the cells of the heart.
Sodium channel blockers: These work by slowing down the electrical conduction in the heart by warding off sodium from entering the cells of the heart.
Procedures for heart arrhythmias
When lifestyle modifications and medications don’t work, certain procedures can help manage and protect against arrhythmias. “The choice of procedure will depend on the mechanisms of the arrhythmia which are typically determined by evaluating electrocardiograms,” says Dr. Latchamsetty.
“Many of the more dangerous forms of arrhythmia occur when the heart has other problems, such as after a heart attack or in the failing heart. In some cases, dangerous arrhythmias become so likely in sick hearts that we prophylactically implant devices called defibrillators, pacemaker-like devices to protect against dangerous arrhythmias that can cause sudden death,” adds Dr. Parker.
Some procedures for arrhythmias include:
Cardioversion: A non-invasive procedure that uses an external defibrillator to send an electric current to your heart to restore normal rhythm
Ablation: A minimally invasive procedure that restores normal rhythm by destroying tissue in the heart that’s causing the faulty signals
Pacemaker: A minimally invasive procedure that implants a small device to send mild electrical pulses to control the timing of your heartbeat and keep it beating normally
Implantable cardioverter-defibrillator (ICD): This minimally invasive procedure implants a small device similar to a pacemaker. It works like a pacemaker and provides a jolt of electricity when a life-threatening arrhythmia, such as V-fib, occurs.
(Here are the 13 things cardiologists won’t tell you.)
Living with arrhythmia
Some heart arrhythmias may improve over time with healthy lifestyle choices such as a heart-healthy diet and exercise. Follow your doctor’s advice and ask what you can and can’t do as far as activities go, and what medications or natural supplements you should avoid. Have a game plan for when symptoms worsen.
If your heart arrhythmia and have a defibrillator or pacemaker implanted, you should carry a medical ID card or wear a bracelet in the event of an emergency. Know the signs of cardiac arrest, heart attack, and stroke. You can monitor some of your vitals at home, but don’t try to diagnose new or changing signs on your own.
(These are the best heart-healthy products for your home.)
“Monitoring for your own arrhythmias can be challenging and an individualized approach including monitoring symptoms and correlating with either taking your pulse or using a personal electrocardiogram recording device can be helpful in some cases,” says Dr. Latchmasetty. She adds, “but such a strategy should be used with the consultation of a medical provider to help interpret the findings and their significance.”
Next, these are the health gadgets that could save your life.