What Is Frontotemporal Dementia? Bruce Willis’ Condition, Explained.
Updated: Feb. 17, 2023
This rare type of dementia comes in many different subtypes, resulting in specific and individualized symptoms.
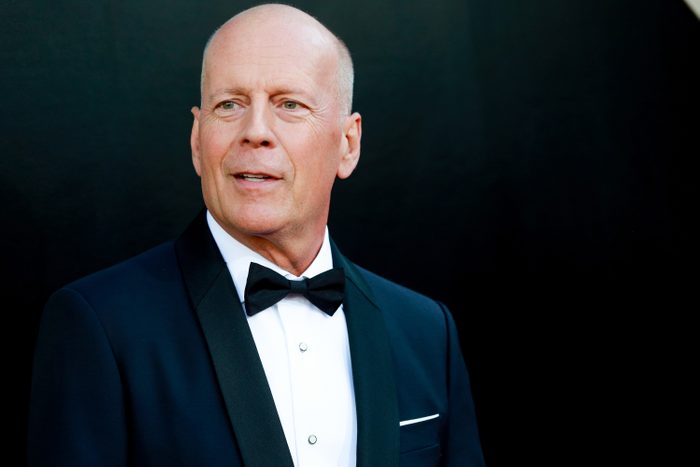
On February 16, 2023, the family of beloved American actor Bruce Willis publicly revealed that he has been diagnosed with frontotemporal dementia. This condition is a more serious evolution of Willis’s aphasia, which the family announced in spring 2022. In their statement, the family says, “While this is painful, it is a relief to finally have a clear diagnosis.”
In the wake of this announcement, fans are wondering what exactly frontotemporal dementia is, as well as what symptoms accompany it, and what treatment can look like. Consider this your basic primer.
What is frontotemporal dementia?
Frontotemporal dementia, otherwise know as frontotemporal disorders or FTD, is a form of dementia. The National Institute on Aging (NIA) explains that it is defined by damage to the neurons in the frontal and temporal lobes of the brain and the Mayo Clinic refers to it as an “umbrella term” for disorders that affect this brain area.
FTD is progressive and degenerative, meaning that its symptoms get worse over time. The neurons in the frontal and temporal lobes will continue to die off, causing these areas of the brain to atrophy.
Unfortunately, FTD tends to affect younger individuals than other forms of dementia do; about 60 percent of those diagnosed are between the ages of 45 and 64. Doctors at the University of San Francisco California’s Center for Memory and Aging claim that within this age demographic, it is about as common as Alzheimer’s. The Mayo Clinic predicts it makes up 10 to 20 percent of total dementia cases.
According to Johns Hopkins Medicine, the exact cause of FTD is yet unknown, though researchers have linked certain subtypes to various gene mutations. For example, some FTD patients have tiny structures called “Pick bodies” in their brain cells, which contain an abnormal amount or type of protein.
The only known risk factor for developing FTD is having a family history of FTD.
What are the signs of frontotemporal dementia?

Symptoms of FTD vary greatly from individual to individual; however, they can be roughly broke down by subtype. The Behavioral Variant (bvFTD) tends to affect behavior and personality, while Primary Progressive Aphasia (PPA) causes difficulty with communication.
Within the PPA category, one subtype—progressive nonfluent aphasia—affects one’s ability to speak, while another—semantic aphasia—decreases the ability to use and understand language. Notably, the Willis family has identified “challenges with communication” as “just one symptom of the disease Bruces faces.”
A rarer form of FTD affects movement and may cause symptoms similar to Parkinson’s or Lou Gerhig’s diseases.
Some early signs of FTD may include the following. The most common are behavioral symptoms, though language or motor difficulties may also develop.
Behavioral symptoms
- Dramatic change in habits, such as a deterioration of personal hygiene or sharp increase in eating
- Difficulty planning or prioritizing tasks
- Apathy or loss of interest in daily activities
- Repetition of the same activity or phrase
- Impulsive, socially inappropriate, or otherwise non-self-aware behaviors
- Distractibility
- Frequent mood changes or increased agitation
Language symptoms
- Difficulty naming objects or understanding meanings
- Increased hesitation when speaking
- Less frequent speech
- Omission of connecting words, such as conjunctions or articles
Movement symptoms
- Tremors or muscle spasms
- Muscle weakness or rigidity
- Poor coordination or balance
- Difficulty swallowing
Because of the similarities in symptoms, FTD may be initially misdiagnosed as depression, schizophrenia, or Alzheimer’s.
Is there treatment for frontotemporal dementia?
As of writing, there are no treatments to cure or slow down the progression of FTD. However, a team of doctors, nurses, and therapists can help anyone who has been diagnosed manage their symptoms. Doctors may prescribe anti-depressants to lessen the impact of psychological symptoms, while speech pathologists may work with the individual to adjust to their new linguistic limitations. If a patient experiences motor difficulties, they can also work with a physical therapist to strengthen weakened muscles.
Fortunately, FTD is not explicitly life-threatening. According to Johns Hopkins Medicine, “people may live with it for years.” While those with FTD are at greater risk of developing pneumonia and other infections, many can still live long, fulfilling lives.
The most important thing for those who know someone with FTD is to accept these new changes, realizing that the individual cannot control them, and to treat the person with dignity and respect. If you would like to support the communities affected by FTD, the Willis family suggests visiting theAFTD.org.
For daily wellness inspiration, get The Healthy @Reader’s Digest newsletter and follow The Healthy on Facebook, Instagram, and Twitter.