Why allergies are out of control
If you feel like you’re having the worst allergy season ever, it’s not just you: More than 24 million people in America have seasonal allergies, and allergists are already reporting that this year is a brutal one for those who experience hay fever allergies. You can blame climate change, as well as a delayed spring in some parts of the country, which is causing everything to bloom all at once. If you’re taking an antihistamine but still feel miserable, you may need to switch up what you’re taking or how you’re taking it, says Tania Elliott, MD, an allergist in New York City, an associate attending physician at NYU Langone Health, and a national spokesperson for the American College of Allergy, Asthma & Immunology (ACAAI). Now, it’s time to pay attention to your body’s signals when it needs better allergy management.

Allergy problem: You have constant sinus headaches
If you have a near-daily headache that pops up the same time each year, chances are, allergies are the trigger. When our body reacts to an allergen, the immune response leaves us inflamed and stuffed up, which can bring on a headache. Allergic headaches tend to be a dull aching, often above your eyebrows and near your cheeks. You may also have post-nasal drip, which happens when your sinuses—normally hollow cavities—get swollen and clogged, leaving the mucus nowhere to go but down the back of your throat. Allergic sinus issues are more than just a hassle—they can set you up for ongoing problems. “Uncontrolled allergies can lead to inflammation and mucus build-up in your sinuses and nasal passages,” Dr. Elliott explains. If you don’t address your allergy symptoms, that swelling can eventually trap bacteria and cause infections. (Here’s how to tell if that headache is actually an allergy migraine.)

Best allergy fix: steroid nasal sprays
Surprise: Steroid nasal sprays (brand names: Flonase, Nasacort) are better than antihistamines at relieving hay fever symptoms in general and sinus woes in particular, Dr. Elliott says. The reason they are ideal, she adds, is they target multiple chemicals that your body produces when exposed to an allergen; antihistamines, on the other hand, only stop one of these chemicals, histamine. Steroid nasal sprays, which are available over-the-counter (OTC), also shrink the swollen tissue inside your nose and sinuses, so snot can drain, and you can breathe. If you’re only using your steroid spray on bad allergy days, you’re using it all wrong: It is a preventative medicine, which means you need to take it every day at the same time for it to work right. Give it five to seven days to kick in, then stick with it straight through allergy season. And avoid the decongestant nasal sprays like Afrin, Dr. Elliott adds, because when taken for more than three days, they can cause rebound congestion, leading to more misery. (Here are more things allergists want you to know this spring.)

Allergy problem: Your eyes are itchy, watery, puffy, or black-and-blue
Do you wake up looking like you’ve been in a fight? Those bruised semi-circles, called allergic shiners, are caused by swelling in the small blood vessels beneath the skin, according to the ACAAI. They usually go hand-in-hand with other allergic eye symptoms such as itching, tearing, and discharge, says Jennifer Caudle, DO, a board-certified family medicine physician and associate professor at Rowan University in Glassboro, New Jersey. It’s all part of your body’s immune response to your triggers—whether that’s something seasonal like birch pollen or a year-round nuisance like cats.

Best allergy fix: Nasal steroids, along with antihistamine eye drops
Yes, an oral antihistamine will help reduce the itch, but a nasal steroid such as Flonase will do more to ease the full constellation of eye symptoms. Use it daily, and it will stem the allergic response and reduce inflammation not only in the nose and sinuses but also around the eyes. If you’re still crazy itchy, add an OTC antihistamine eye drop as needed. A word of warning: Avoid the redness-reducing eye drops (like Visine), which will do zip for your allergies and make your eyes look even redder. That’s because these drops constrict blood vessels in the eye to reduce redness temporarily, and when you stop using them, you get rebound red-eye. Deceptive labels trick many smart people into buying them, Dr. Elliott warns: “Some say on the label that they’re for allergies when they’re not.” Steer clear of products containing oxymetazoline, the ingredient that shrinks blood vessels.

Allergy problem: Your asthma is acting up out of the blue
Breathing in pollen and other allergens can trigger chest tightness, coughing, wheezing, and shortness of breath, all telltale signs of allergic asthma, says Murray Grossan, MD, an ear, nose, and throat doctor in Los Angeles and author of The Whole Body Approach to Allergy and Sinus Relief. In addition, if you get chronic asthma, eczema, and seasonal allergies, you may have a genetic allergic condition called Atopy, he says. “When you have eczema, allergies and asthma together this can lead to heightened immune responses to common allergens like pollen and food. This needs to be treated and managed or it can cause serious problems,” he explains.
You can’t count on your usual allergy drugs to help. “Nose sprays and antihistamines do not treat asthma,” Dr. Elliott says. Frequently needing your rescue inhaler (which contains a medication such as albuterol) is a flashing neon sign that you need a better asthma treatment plan. (These are the 6 asthma symptoms adults should never ignore.)

Best allergy fix: Inhaled steroids
Experts now know that when asthma isn’t properly controlled, the swelling and spasming in the airways can get worse and potentially cause long-term damage to the respiratory system. “I can’t stress enough that if you have spring allergies, you shouldn’t be on as-needed rescue inhaler; you should be on every day steroid inhaler,” says Dr. Elliott. “You don’t want to let it get out of control, because then it snowballs into an asthma exacerbation.” Book an appointment ASAP with an allergist or pulmonologist, who can prescribe a steroid inhaler, such as Flovent. You need to use these steroid inhalers every single day for them to work. And if that doesn’t make you feel much better? In some cases, allergists will prescribe a pill called Singulair for allergic asthma. It controls leukotrienes, a chemical in our body that triggers some but not all cases of allergic asthma. It only works 25 to 50 percent of the time, however, and can have side effects, so it isn’t usually a first-line treatment.

Allergy problem: You’re. So. Tired.
It’s beautiful out but instead of feeling pumped, you feel pooped. Allergies may be the last thing you suspect, but don’t overlook them, Dr. Elliott says. In fact, before she became a doctor, she used to feel exhausted around the same time each year and didn’t know why. “Every summer in August, I would feel so tired. I was drinking more and more caffeine, but I had a tired and foggy feeling,” she says. Once she got diagnosed with ragweed allergies and treated them, she stopped feeling zonked—and she found her calling to become an allergist. (Here’s how allergy symptoms may be hijacking your work day.)
Here’s how allergies leave you drained: When your body encounters an allergen, it mounts an immune response, just as if you were exposed to a virus. That reaction takes energy. Not to mention, allergies disturb your sleep, as the nasal passages can get so congested that you end up mouth-breathing. Allergies can even lead to sleep apnea, a condition in which you wake up repeatedly during the night because you’re not getting enough oxygen. It’s treatable, but it’s a risk factor for heart disease, so be sure to see a doctor.
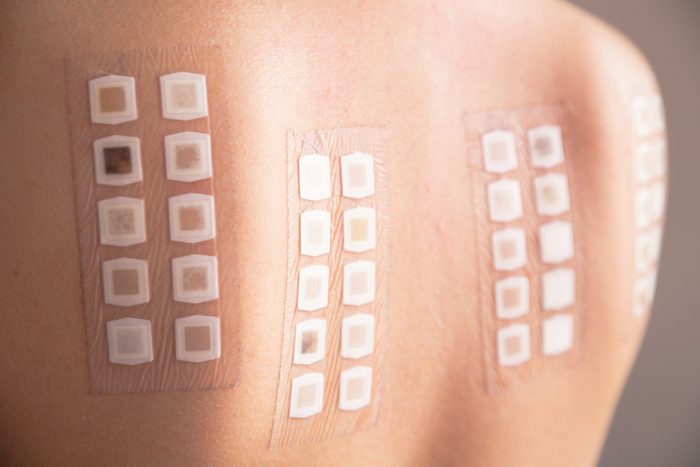
Best allergy fix: allergy testing and immunotherapy
If you have spring lethargy, check in with an allergist and ask for testing, Dr. Grossan says. Once diagnosed, you’ll likely be put on a steroid nasal spray (which will make it easier to breathe at night) as well as an antihistamine. Another option is allergy shots, which have a cure rate of 75 percent. A form of immunotherapy, allergy shots involve injections of tiny amounts of the things you’re allergic to under the skin on a weekly basis at first, then less frequently. The shots help train your body to tolerate the offenders. If you’re allergic to ragweed, grass, or dust, you can skip the needles and take an immunotherapy pill instead. Oral immunotherapy is much less of a time commitment because you can take the pills at home. Still, going the oral route can give you an itchy throat, which is one reason why Dr. Elliott isn’t sold on it: “I think it’s gross to eat dust.” (Find out how allergists control their own allergies.)

Allergy problem: You have brain fog
Raise your hand if you’ve been feeling spacey, forgetful, or unable to concentrate lately. It could be due to allergies, Dr. Caudle says. It’s not totally clear how allergies cloud your thinking, but experts think it’s a result of your immune response, lack of restful sleep, and the side effects of antihistamines, which can leave you groggy. Studies have even shown that worker productivity slips during allergy season.

Best allergy fix: Start your meds before allergy season hits
The sooner you get your allergies under the control, the better you’ll feel. That means if you have grass allergies, which hit in summer, you should start taking your meds in spring. “Take the medication exactly as prescribed and don’t skip doses, you want the medications to be in full effect before the season gets going,” Dr. Caudle advises. Once the inflammatory process is underway, it’s harder to control. (Here are 11 more things you’re doing that could make your allergies worse.)

Allergy problem: You have hives or a rash
It’s not super common to break out in hives and rashes from pollen allergies (hives are more common with food allergies), but it happens. “If you’re allergic to grass and you’re rolling around in it, you could definitely get a rash or hives,” Dr. Elliott says. And people prone to eczema—a condition caused by the breakdown of the skin barrier—are more likely to get flares during allergy season.

Best allergy fix: Baby your skin
If you’re planning on hitting the trails or lazing in the grass, wear long pants and sleeves, Dr. Grossan says. Get gloves for gardening. If you do notice hives, pop an antihistamine to ease the itching. As for eczema, “it’s a breakdown of the skin barrier, so a good moisturizing regimen is really important,” says Dr. Elliott. She suggests taking a shower and then immediately applying Vaseline, which acts as a barrier to protect the skin. At the first sign of a flare, treat it with a bit of an OTC low-dose steroid cream. (Don’t miss these 13 skin allergy myths you need to stop believing.)

Allergy problem: You can’t stop sneezing and sniffling
So you’re on three different allergy drugs and you still feel wretched? It’s only normal to ask your doctor (or “Dr. Google”): “Has my body built up tolerance to my antihistamine?” But the truth is, that’s an urban legend, Dr. Caudle says. “One of the biggest signs I see that a patient’s allergy meds are not working well for them, is that they still have symptoms despite properly taking their medications,” she says.” Some also complain of some improvement in symptoms but not total symptom resolution with taking their medications. This is what tells me that we need to rethink our allergy treatment strategy.”

Best allergy fix: Extra antihistamines
A solution in your allergist’s bag of tricks: Upping the dosage of antihistamines such as Zyrtec. “We treat with a high dose—we’re not afraid to up the ante,” Dr. Elliott confides. Sometimes that means taking it twice a day instead of once, or taking two pills, morning and night. Make sure to consult a doctor before bumping up the dosage of any drug. (Never, ever take higher doses of Benadryl; that could be dangerous.) Another option is to try switching antihistamines. While there’s no research proving it will help, there’s no harm in trying it, as long as you stick with second-generation antihistamines (Allegra, Zyrtec, Xyzal, Claritin) and stay away from Benadryl, which is sedating. Lastly, avoid your triggers and take measures to get rid of them: Wash your hair every night. Take off your clothes as soon as you get in the house and wash before wearing again. Rock big sunglasses to protect your eyes. And here’s a weird one: Avoid hairspray and gel, Dr. Elliott says, because they cause pollen to cling to your strands. If you feel an attack coming on, follow these tips to stop any allergy attack in its tracks.
