I Almost Died From a Heart Attack Because of a Little-Known Type of Cholesterol
Updated: Mar. 11, 2022
With a total cholesterol level in the healthy range, one man thought he was OK—until he almost died of a heart attack. Here's how lipoprotein(a) played a role—and why you should pay attention to your LP(a) level.
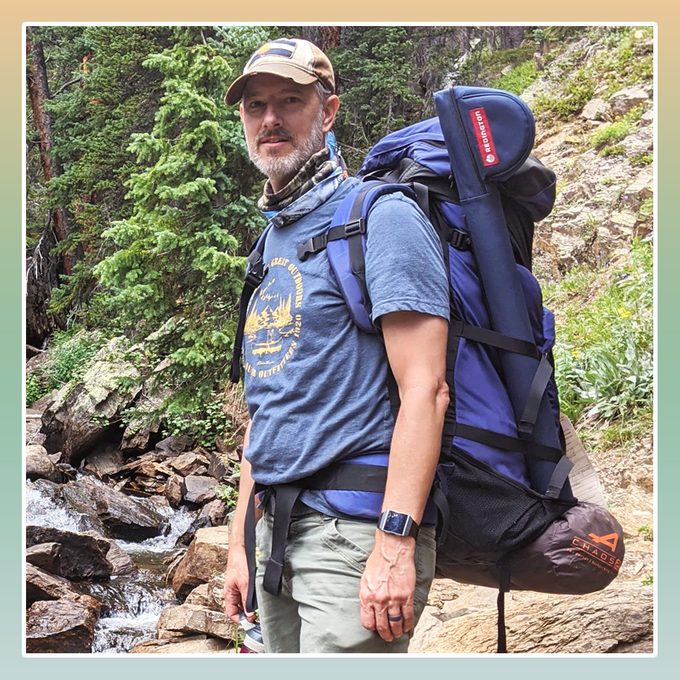
High cholesterol doesn’t cause symptoms, but that doesn’t mean it’s harmless. In reality, the condition increases your risk for heart disease and stroke. High cholesterol is defined as having a total blood serum cholesterol 240 mg/dl or over. Borderline high cholesterol happens when your cholesterol levels fall between 200 mg/dl and 239 mg/dl—and it affects nearly 40 percent of American adults. But your total cholesterol doesn’t tell the whole story. It’s important to know your LDL (low-density lipoprotein, the “bad” cholesterol), HDL (high-density lipoprotein, the “good” cholesterol), and triglycerides. Now there’s a new number you should pay attention to, particularly if you have a family history of heart disease: lipoprotein(a), or LP(a), a particle that is a part of LDL cholesterol. Mike F., 50, a married father of four and a marketing professional in Denver, shares how learning about this number saved his life.
I track my cholesterol on a spreadsheet—here’s why
I have an Excel spreadsheet listing all my cholesterol data for nearly two decades. That may sound extreme, but those numbers have come to affect nearly every aspect of my life.
When I was first diagnosed with high cholesterol, I had no idea that I’d soon become an expert on it or that my very life would depend on me learning everything I could about the genetic influences on high cholesterol and how it causes heart disease.
Typical treatment for typical high cholesterol
In 2004, I was just 33 years old—and slim and fit. But I did work an extremely stressful job, and I knew that high cholesterol ran in my family.
So I wasn’t too surprised when a routine checkup showed high LDL cholesterol, low HDL cholesterol, high triglycerides, and a total cholesterol number near 300 mg/dl. (Ideally, total cholesterol should be under 200 mg/dl.)
My diet wasn’t great, and I knew there were some things I could be doing to improve my health. But I was a young dad in a demanding job, so I made half-hearted changes. I first tried to lower my cholesterol by taking fish oil supplements and exercising more.
That didn’t do the trick, so my doctor put me on a prescription statin medication. This helped immensely.
I took various statins for the next 13 years, and since my total cholesterol number was consistently in the healthy range, I assumed everything was fine.
Sudden, unexplained pain
In October 2017, I was on the StairMaster at the gym when I suddenly got a sharp pain in my back, between my shoulder blades. It was so intense that I got off the machine to loosen the muscles with foam rolling and stretching.
Thankfully, the pain subsided. A pulled muscle, I thought.
But then it happened again the next day, and the next.
By the fourth day, I began to recognize a pattern: Whenever my heart rate became elevated, hitting my workout zone, the pain appeared. When my heart rate dropped, the pain receded.
Still, I wasn’t too worried, as upper back pain isn’t a typical symptom of a heart attack, and I didn’t have any other signs. Plus, all my blood work was great, so I had nothing to worry about, right?
Wrong. On the fifth day, I got the back pain during my workout. This time it was accompanied by extreme sweating, tingles in my left arm, and chest pain. After a restless night, I went in to see my doctor.
She did an EKG, which was normal, and took some blood. She told me it was probably just heartburn, wrote me a prescription for an antacid, and sent me on my way.
A nearly fatal heart attack
A few hours later, she called me with the results of my blood work and the prognosis was dire: I was having a heart attack and I needed to go to the hospital immediately. None of my family members were around, so I drove myself to the ER, where doctors admitted me right away.
Scans showed a 90 percent blockage of my left anterior descending artery (LAD). It’s the largest coronary artery, and a block there is called a “widow-maker” because it is so often fatal.
I had cardiac surgery, during which a surgeon put a stent in my artery to widen the previously blocked pathway and allow for blood flow. My wife and I consider ourselves very fortunate that we caught my heart attack before it lived up to its terrifying name!
But while the surgery solved the immediate problem, it didn’t answer the question of why I’d had a heart attack in the first place when my cholesterol was under control and I had very few risk factors.
My lipoprotein (a) level was very high
The answer lay in a number I’d never heard of before: lipoprotein(a). The LP(a) particle is part of LDL cholesterol—you know, the bad stuff that’s associated with heart attacks.
When I first started tracking my cholesterol, my doctor noted that my LP(a) was high. But back then, not enough was known about lipoprotein(a) to draw any conclusions.
Fast forward more than a decade. New research has found that LP(a) is highly influenced by genetics, rather than lifestyle factors. It has a high correlation with heart disease, even if other cholesterol numbers are in the normal range.
After my heart attack, my doctors noticed that even though my total cholesterol was normal, my LP(a) was still extremely high. A normal LP(a) is around 30 mg/dl and no more than 50 mg/dl. Mine was 246 mg/dl at the time of my heart attack.
The bottom line: my cholesterol wasn’t too high according to traditional lipid recommendations, but it was too high for my body.
A new normal
After having a heart attack and learning about the genetic risk reflected in my LP(a) level, I knew I had to take serious steps to lower my cholesterol.
My doctor put me on evolocumab (Repatha), a type of cholesterol-lowering medication that targets hereditary heart disease. I inject it every two weeks. In addition, I take a daily prescription statin, a blood thinner, and aspirin.
Even though my risk for heart problems is largely genetic, I wasn’t going to add to the likelihood of another heart attack by following an unhealthy lifestyle. So I overhauled my diet.
I was advised to limit my intake of saturated fat to less than 12 grams per day, so I had to cut out many of my favorite foods, like hot dogs, red meat, dairy, and cake frosting.
My fitness routine needed a boost too. I increased my exercise to at least 45 minutes of cardio four to five days per week.
I also did everything I could to lessen the stress in my life, including moving to a quieter city, taking a less-demanding job, prioritizing time with my family, and spending time on my favorite hobbies: hiking, camping, and biking in the Colorado mountains.
Positive changes
For someone who had a nearly fatal heart attack, I’ve had a miraculous recovery. I have no lasting heart damage, and I’m able to do all the activities I enjoy with no restrictions.
Even more shocking, though, are my cholesterol numbers. My total cholesterol is now 69 mg/dl. My LDL is 16 mg/dl. And my triglycerides are in the 30s. (Yes, you read those numbers correctly!)
But those numbers don’t tell the whole story. My LP(a) is currently around 160 mg/dl. That’s much better than it was before, but it is still considered dangerously high, and I’m working with my doctor to lower it.
It’s tricky, though. While scientists know a lot more about LP(a), there’s still so much more they need to learn about it and how to treat it. This is why I enrolled in a clinical trial that’s studying LP(a), genetic high cholesterol, and its effects on the body.
Participating in this research and sharing my story is so important to me. I want to educate others about the importance of knowing their LP(a) and not just relying on the standard cholesterol numbers.
But it’s also very personal. There’s a good chance I’ve passed down my genetic susceptibility to heart disease to my four kids. And I’m going to do everything in my power to make sure they don’t have a heart attack in their 40s like I did.
—As told to Charlotte Hilton Andersen