My Doctor Told Me Not To Worry About My High Cholesterol—and I Ended Up Needing a Quadruple Bypass
Updated: Sep. 07, 2021
Here's how one woman found a treatment for her genetic high cholesterol after a healthy lifestyle, statins, and a controversial heart test didn't help.

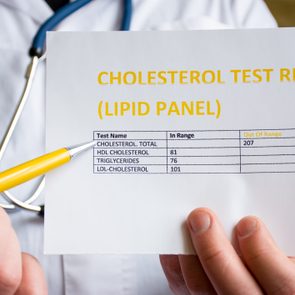
High cholesterol
High cholesterol is nothing to ignore. After all, it raises your risk of heart disease and stroke. There are a lot of things that can cause high cholesterol: a lack of exercise, an unhealthy diet, smoking or other lifestyle factors, certain medication, a chronic illness, or an inherited genetic mutation. It’s important to determine the true cause of your high cholesterol so you can find the best treatment for your case. Therese Roth, 61, a medical researcher in Ann Arbor, Michigan, shares how she finally found an effective treatment for her genetic high cholesterol after lifestyle changes and a controversial heart test—a coronary calcium scan—didn’t work for her.
My family is no stranger to heart disease
I have always known I was at high risk for heart disease. My mom had a quadruple bypass heart surgery when she was just 54 years old. And she’s not the only one.
My mom’s branches of the family tree include many people who died too young from heart disease. I was determined to not be one of those cases, so I’ve always been mindful of how I cared for my heart. And that has meant watching my cholesterol.
High cholesterol certainly played a part in my mother’s heart disease—her cholesterol levels were not well controlled. I also believe many of my relatives had genetically high cholesterol, although I can’t verify it because these things weren’t tracked back then the way they are now.
So when I was diagnosed as a young adult with high cholesterol, I wasn’t surprised. And at first I wasn’t too worried. I was already living a very heart-healthy lifestyle, so I thought I could manage my high cholesterol on my own.
I did everything right, but my cholesterol was still high
Throughout my adult life, I exercised regularly, did not smoke, rarely drank alcohol or soft drinks, and seldom ate fast food. I was a competitive powerlifter and still work to encourage women to do strength training.
My healthy lifestyle certainly helped. My HDL (“good”) cholesterol and triglycerides were good, and my total cholesterol was only borderline high.
Unfortunately, as I started to get older, my LDL (“bad”) cholesterol levels continued to rise—despite my healthy lifestyle. Eventually, my doctor recommended that I start taking cholesterol-lowering medication.
I followed my doctor’s orders and took statins for years, yet my high cholesterol kept getting higher. I tried different brands of the drug, but the statin side effects were terrible. They all made my muscles hurt, and I was easily fatigued.
I was referred to a nutritionist, who wanted me to try dietary changes. The problem: my diet was already very heart healthy, so there wasn’t much left to try. I even went vegan for a month, but my cholesterol numbers still increased.
None of the usual treatments for lowering LDL cholesterol were working, and I was concerned about the potential effects on my health.
A controversial cholesterol test gave me the all clear
I received a referral to an internal medicine doctor who specializes in hard-to-treat cholesterol cases. Because medication and lifestyle changes had failed to reduce my cholesterol, he suggested I get a coronary calcium scan (CCS).
This is a specialized, rapid X-ray scan that takes pictures of your heart to detect and measure calcium-containing plaque in your arteries. The calcium deposits are given a number, called an Agatston score, which ranks the severity and determines your risk of a future heart attack.
The higher the Agatston score, the higher your risk. A zero means that the scan detected no buildup in your arteries, and you have a very low chance of developing a heart attack in the future. A score of 100 to 300 is a moderate risk, and anything over 300 is considered a very high risk.
My score was zero.
The doctor told me that this meant I had no calcium blockages in my coronary arteries and I didn’t need to worry as much about my high cholesterol numbers. He even said I could go off my statin medications until my next scheduled scan in five years. I was delighted!
The CSS is often touted as a way to measure plaque buildup, but there is some controversy in the medical community surrounding its use.
Current guidelines from the American Heart Association (AHA) state that it is a useful test for people who fall in a cholesterol gray area because it helps determine if they need medical treatment. But the AHA recommends against using it alone, viewing it instead as just one of several factors used to determine appropriate treatment.
At my doctor’s advice, I went off my meds
I stopped taking cholesterol medication, as my doctor had suggested, and continued living my healthy lifestyle.
My doctor had cautioned me that no test is 100 percent accurate, saying I should still be on guard for any symptoms that could indicate cardiac problems. It was a prescient warning.
Three years after I stopped my medications, I started feeling a pinching sensation in my shoulders after walking up stairs. And heat really started bothering me.
I recognized these as possible symptoms of a serious heart problem.
I ended up needing quadruple bypass heart surgery to save my life
I went back to my doctor, who recommended a stress test, just to be safe. Abnormal results from that led to a referral to a cardiologist and additional heart testing.
The cardiologist discovered that I had many blockages along multiple coronary arteries—too many for stents.
The surgeon immediately scheduled me for a quadruple bypass.
I was only 59 years old and very active, so the prospect of open-heart surgery was more than a little daunting. Thankfully, my surgeon, nurses, and other members of the team were all amazing. I also had the full support of my family and many loved ones.
The surgery was successful, and I made a full recovery. In fact, it was so successful that I was able to return to powerlifting. I actually competed in the sport the year following my quadruple bypass, increased my own personal best lifts, and even set three new state records in my age and weight class.
My focus shifted to treating the genetic cause of my high cholesterol
After my bypass, I continued to have high cholesterol, which indicated that it might be caused by a genetic mutation.
My cardiologist recommended a PCSK9 inhibitor, which is an injectable drug that reduces cholesterol in a different way than statins do. Doctors generally use it to address high cholesterol caused by a genetic mutation.
We discovered that I have the heterozygous familial hypercholesterolemia, or HeFH mutation. It’s a rare genetic condition that can lead to soaring LDL cholesterol and heart problems at a young age. And it explains why this medication worked when nothing else had.
I have to inject the medication every two weeks, and after just three injections my LDL cholesterol dropped by almost 80 percent. Not only did it work to lower my cholesterol, but I haven’t experienced any side effects either.
For over two years, I have been on the PCSK9 inhibitor, plus a low-dose statin to reduce inflammation, a baby aspirin, a triglyceride-reducer, and a beta-blocker. My cholesterol is finally well controlled.
I have not had any further heart problems, but I wish we had realized earlier the true hereditary cause of my high cholesterol. Lifestyle changes alone couldn’t treat it, and if I’d started a PCSK9 inhibitor earlier, I could have saved myself a lot of pain and frustration—and possibly open-heart surgery.
My greatest advice: know your risk factors
High cholesterol often gets a bad rap for being the result of eating junk food and not exercising enough. And, yes, those are some pretty big risk factors.
But there are many causes, including genetics. Finding out the root cause of your high cholesterol is so important because it determines what treatments and interventions will work. Not everyone responds the same way to different treatments, so doctors and patients need to work together to find what works best (and with the fewest side effects) for each individual.
This is also why it is so important to know your family history of heart disease and share it with your children.
After my experience, I made my children get their cholesterol checked right away. My doctor informed me that genetically high cholesterol would be evident before age 20, so it was important they get tested as soon as possible. If it was high, they’d need to start treatment right away.
Regardless of your history, you should know your baseline cholesterol level so you can watch how the numbers change over time.
This will help you start interventions right away, before damage is done to your arteries. You do not want to end up needing open-heart surgery if you can avoid it. Take it from me.
—As told to Charlotte Hilton Andersen