Swayback vs. a Hump: The Difference Between Lordosis and Kyphosis
Updated: Mar. 11, 2022
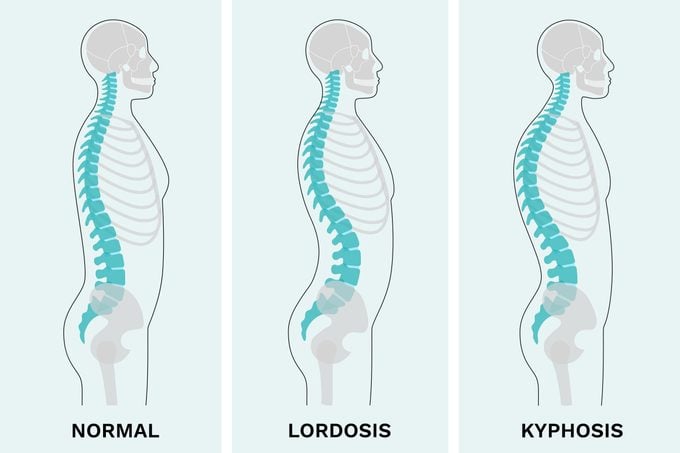
Kyphosis and lordosis are normal curves in the spine. Both can cause issues when they're excessive, but one has the potential to be more troublesome, causing back pain and other symptoms.
Kyphosis vs. lordosis
A quick look at your back will tell you that your spine curves, at least a little bit.
Normally, your spine will curve inward in the neck (cervical) and low-back (lumbar) regions, a curvature called lordosis. The outward curvature of your spine, specifically in the upper and mid-back (thoracic region), is called kyphosis.
Both of those curves are totally normal.
“It is only when these curves are excessive that we have a problem,” says Joseph Davey, MD, chief of pediatric orthopedics at the University of Oklahoma in Oklahoma City.
Abnormal spinal curves may make you automatically think of scoliosis. And, indeed, that type of curvature does deviate from the norm. But unlike kyphosis and lordosis, scoliosis is an abnormal sideways curve of the spine.
Excessive lordosis, however, may make your back extra flat or cause your butt and belly to stick out, while excessive kyphosis can lead to rounded shoulders.
Here’s how to spot the curves of kyphosis and lordosis and what to do to treat the spinal conditions.
Can you have both lordosis and kyphosis?
Lordosis and kyphosis can occur together—and that’s a good thing.
“We should always have both,” says Dr. Davey.
A certain amount of curvature in the lumbar and thoracic spine is essential to preserve the balance between internal and external forces. It’s how we keep our head and trunk over our pelvis and maintain internal forces created by muscles.
Essentially, lordosis, kyphosis, and our pelvic tilt work together to keep us upright.
“If the spine was just straight [looking from the side], it would be leaning forward,” says Dr. Davey. “The most normal, balanced position is to have our center of gravity over our pelvis.”
When these two curves are out of balance, typically when you have excess upper spine kyphosis or reduced lower lordosis, you can experience pain.
What is lordosis?
Lordosis is an inward curve of the lower spine and normally nothing to worry about—it’s natural to have some degree of curvature specific to how our body is structured.
Normal lordosis helps our body absorb weight and impact as we go about our day, whether we’re walking, getting out of a chair, or pounding the pavement during a run.
A certain amount is essential so we can stand up straight and have good posture.
As we get older, the curves can worsen. Some people may develop bad posture or spinal deformity, have pain, or experience difficulty walking.
When the lower spine becomes too curved, it’s called hyperlordosis, or swayback. When the lower spine is too straight, it’s called hyperlordosis, or flatback.
What causes swayback?
Hyperlordosis can develop at any age, but it tends to happen in adolescence. It’s often linked with one of the following:
-
Poor posture: Weak abdominal muscles struggle to support the lumbar spine.
-
Being overweight: Extra belly fat puts strain on the lower back and pulls it forward.
-
Trauma: Accidents or sports injuries can cause stress fractures that, if left untreated, may lead to spondylolysis. With this condition, the vertebrae slip out of alignment with the rest of the spine.
-
Achondroplasia: A common type of dwarfism.
-
Neuromuscular conditions: Certain conditions weaken nerve and muscle function, such as muscular dystrophy and cerebral palsy.
-
Congenital problems: These can affect the vertebrae
-
Arthritis: This may result in flatback syndrome.
- Osteoporosis: The bone disease osteoporosis causes weak, thinning bones and may lead to lordosis.
Signs and symptoms of lordosis
Here’s some good news: “Lordosis rarely causes any problems,” says Dr. Davey.
It’s more common to have pain if the spine is out of balance from excess upper-spine kyphosis or reduced lower lordosis.
“People with a flat back due to arthritis or other causes tend to lean forward and have pain,” he adds.
In more severe and untreated curvatures, lordosis might cause the following symptoms:
-
Pain in the lower back
-
Difficulty moving about while doing daily activities
-
More prominent buttocks and tummy
-
A large gap between the floor and the lower back while lying on a hard surface
-
Back pain when standing in one place for prolonged periods
-
Fatigue and neck discomfort
How is swayback diagnosed?
There’s a relatively wide range of normal lordosis in the lower back. That makes diagnosing it a bit tricky—what’s normal for one person may not be normal for another.
Your doctor may do a physical examination to gauge the extent of your curvature. If your back isn’t very flexible or there is pain, you may need X-rays to determine the cause of your issues.
And if you feel tingling, numbness, muscle spasms, pain, or weakness in your arms or legs, or experience changes in your bladder or bowels, your physician may recommend a neurological assessment.
Does swayback need to be treated?
In most cases, swayback is more of a cosmetic concern than a functional alignment problem.
Provided your back is still flexible (that is, you can still bend forward without issue), you probably won’t need treatment.
Still, your doctor may elect to keep an eye on the curve at routine checkups.
If you have pain, limited flexibility, or other symptoms, you may require one of these treatments:
-
Over-the-counter (OTC) nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain
-
Physical therapy to improve range of motion and build strength and flexibility
-
Exercises to instill better posture and strengthen the core and back muscles
-
Weight loss in the belly area to improve posture and decrease the curvature

What is kyphosis?
Kyphosis is a forward bending of the spine, which leads to a round back (a hump, or hunchback).
The average spine will curve outward in the upper mid-back region, so how do you know whether your curvature is normal or not? It can be hard to tell.
The range of normal kyphosis is fairly broad, falling between 10 and 40 degrees.
“Mild excess kyphosis is not usually a big problem,” says Dr. Davey. “If it continues to worsen or leads to back pain, we are more concerned. If kyphosis reaches 80 degrees, surgery may be needed.”
Types of kyphosis
Kyphosis can occur as a deformity in the womb, but it is most often seen in growing children. That said, it can still occur in adults.
The four primary types of kyphosis are postural kyphosis, congenital kyphosis, Scheuermann’s kyphosis, and age-associated kyphosis.
Postural kyphosis
The most common form of kyphosis has to do with posture.
Slouching, carrying a heavy backpack, or otherwise practicing poor posture can stretch the muscles and ligaments that hold the vertebrae in place. Out-of-whack vertebrae can create a rounded shape in the spine.
The curve in this kyphosis is flexible, which means it can be minimized with good posture and exercises.
Congenital kyphosis
Congenital kyphosis occurs in the first six to eight weeks of fetal development, resulting in a malformation in the shape of one or more vertebrae.
It can cause the spine to develop a sharp forward angulation as it grows. This curve is visible when looking at the back.
The curve may become larger and more noticeable within the first year of life and can worsen as a child grows. Frequent medical observation is necessary since surgery is sometimes a necessary solution.
Scheuermann’s kyphosis
Scheuermann’s kyphosis, also known as developmental kyphosis, emerges when the bones of the spine in the middle of the back curve outward more than they should.
The curve in this type is rigid, so changing position and adjusting your posture, doesn’t make the hump disappear.
It happens to about 3 percent of kids ages 10 to 15 and is much more common in boys.
This type of kyphosis usually doesn’t cause too much concern because most kids outgrow it when their bones are done growing.
Age-associated kyphosis
Age-associated kyphosis is directly associated with the natural aging process.
Our spines age with us, so as we get older we may develop conditions that lead to kyphosis.
“The kyphosis in aging adults can be from either disc degeneration, arthritis, or even compression fractures from osteoporosis,” says Tenner Guillaume, MD, a pediatric spine surgeon and chief of staff at Gillette Children’s Specialty Healthcare in Saint Paul, Minnesota.
Over time, fractures and osteoporosis weaken the vertebrae, causing them to narrow and shrink.
“This is often why older folks get shorter and more hunched with age,” says Dr. Davey.
Age-associated kyphosis can prompt more aches and pains and make mobility difficult, raising the risk of falls and fractures.
Kyphosis causes and risk factors
While some types of kyphosis develop in the womb, others result from acquired conditions such as:
-
Neuromuscular disorders
-
Spina bifida
-
Osteoporosis
-
Genetics
-
Spinal injury
-
Aging spine (disc degeneration, arthritis)
-
Spine fractures
Signs and symptoms of kyphosis
Depending on your degree of kyphosis, you might not have any aches, pains, or difficulty moving your back.
But excessive kyphosis puts added stress on the muscles and joints of the spine and often results in pain.
Depending on your type of kyphosis or the conditions associated with your kyphosis, you may have additional symptoms beyond pain.
Here are the most common signs and symptoms of kyphosis:
-
Poor posture
-
Rounded back
-
One shoulder blade higher than or protruding more than the other
-
Head noticeably bent forward from the rest of the body
-
When bending forward, the upper back appears higher than normal
-
Hip problems (tight hip flexors)
-
Mild pain or stiffness in the back and shoulder blades.
-
When the kyphosis is due to an accident or injury, severe pain in the back and shoulder blades, with additional symptoms related to the injury
-
Difficulty walking, pain in the legs, and difficulty controlling the bladder (with congenital kyphosis)
How is kyphosis diagnosed?
When it comes to children, it’s always best to get an early diagnosis. There are more nonoperative treatment options available while the bones are still growing.
Sometimes a parent will notice a roundness of the upper back, pointing it out to their child’s doctor. Other times, a doctor might spot the hump during a checkup.
The standard protocol for diagnosing kyphosis in adults and children begins with a medical history, physical examination of the spine, and an X-ray of the spine.
If the curvature is severe, a doctor may order an MRI to see if the curves affect the lungs or spinal cord.
Older adults may need additional tests to see if the kyphosis is related to other existing conditions, such as degenerative disc disease or osteoporosis.
How is kyphosis treated?
If treatment is necessary, your doctor will consider your age, medical history, type of kyphosis, and the size of the curve before creating a plan to care for your kyphosis.
In children, the goal is to stabilize or stop the curve from getting worse. If the curvature needs treatment, the options include:
Regular checkups
Often, you might not need treatment right now. In that case, your doctor will continue to observe the curvature via regular checkups. Children may get X-rays of the spine to monitor the curve’s progress during the growing phase.
Nonsurgical options
Nonsurgical methods are highly successful in treating kyphosis. Physical therapy is the go-to method of treatment.
Exercises can help improve posture and strengthen the core and back muscles. Specific exercises can stretch tight hamstring muscles and soothe aches and pains.
(By the way, physical therapy is the mainstay treatment for scoliosis too)
OTC meds
If you experience pain related to your kyphosis, you may need to take NSAIDs as needed. These OTC meds are effective for relieving minor back pain.
Back brace
Your doctor might suggest wearing a brace, but this type of therapy isn’t customary.
The exception is for children who have Scheuermann’s kyphosis.
“If [curvature is] over 55 degrees or painful, bracing may be an option and has been shown to be effective at altering natural history—but only in children with growth remaining,” says Walter Truong, MD, a pediatric orthopedic surgeon at Gillette Children’s Specialty Healthcare in Saint Paul, Minnesota, and assistant professor in the Department of Orthopaedic Surgery at the University of Minnesota.
Bracing isn’t effective, however, once a child is done growing.
Adults may get some pain relief from intermittent bracing and physical therapy, but the brace won’t correct the curvature in a person who has reached skeletal maturity.
Surgery
The majority of kyphosis conditions are managed with nonoperative options such as physical therapy.
Surgery is reserved for people with severe back pain, spinal deformity, or decompression of nerve roots. In congenital kyphosis, surgery is performed before the curvature gets too large with a goal of effectively halting the growth of the curve.
Posterior spinal fusion surgery is the gold standard for flexible deformities. Fixed deformities often require more complex surgery.
Next, learn about the symptoms of scoliosis in kids and adults.




















