What Is Skin Writing? Everything You Need to Know
Updated: Jul. 06, 2021
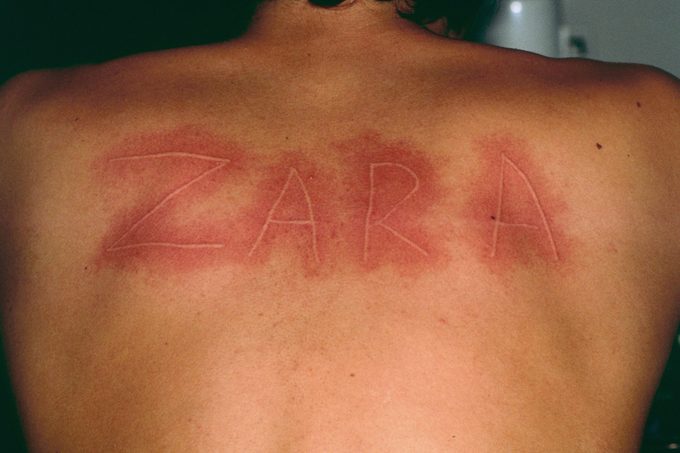
Red, raised, itchy, and swollen skin from light touch can be a sign of dermatographic urticaria—aka skin writing. Here's what to know about this allergy-like condition.
What is dermatographic urticaria?
Scratch your skin hard enough, and you’ll notice red, raised, itchy, and swollen marks. That’s a normal reaction.
But if you have dermatographic urticaria, a condition referred to as skin writing, you won’t have to scratch so hard to get a reaction. Even moderate pressure or irritation can trigger an exaggerated response.
Allergy-like symptoms, such as minor, temporary skin flares or swelling can develop and last more than just a few minutes.
In some cases, people with the condition can break out in hives, round, raised, itchy, red, or skin-colored bumps that blanch, or become white in the middle when pressed.
In some cases, this response is no more than bothersome and uncomfortable. But in rare cases, it can be severe enough to interfere with daily life.
Here’s everything you need to know about dermatographic urticaria, including causes, symptoms, treatment options, and prevention tips.

Why is it called skin writing?
Dermatographic urticaria answers to a few different names: dermatographia, dermatographism, dermographism, and, of course, skin writing.
The term “dermatographism” literally means “to write on the skin.” The condition gets its nickname from the lines or patches of hives that develop on the skin when it is scratched, rubbed, stroked, or when pressure is put on it.
“Dermatographism means skin writing because you could actually take your fingernails and write on someone’s skin,” says Joseph Jorrizzo, MD, and professor of dermatology at Wake Forest University School of Medicine in Winston-Salem, North Carolina.
What causes skin writing?
Dermatographism is caused by an abnormal or excessive release of histamine, a chemical released by immune cells that triggers allergic reactions, including hives.
When specialized immune cells called mast cells detect allergens, they release histamine into the body. They may also release it if they detect a lot of pressure.
Histamine causes blood vessels to widen, or dilate, and causes small blood vessels to leak fluid into the skin, causing edema, or swelling.
Simple dermatographism is not itself considered to be an allergy, says Dr. Jorizzo. It’s just an exaggerated reaction. The mast cells release histamine when there are no allergens present.
Symptomatic dermatographism, on the other hand, leads to actual allergic responses, such as hives.
“Symptomatic dermatographism is a true, physical allergy mediated by an immune response,” he explains. “In cases of simple dermatographism, it seems mast cells are simply more sensitive to pressure than normal.”
How common is dermatographic urticaria?
About 25 to 50 percent of people develop a minor red streak or skin flare and swelling when the skin is strongly pressed, stroked, scratched, or rubbed, according to DermNet NZ, a dermatological site supported by the New Zealand Dermatological Society.
In these cases, symptoms typically go away pretty quickly, often within minutes.
When the response to skin pressure or irritation is exaggerated (and prolonged) enough, it’s considered dermatographism.
“In around 7 percent of people, if you apply a standard pressure to the skin of their back, [they] develop an exaggerated wheal (raised, itchy patch of skin) and flare reaction,” says Dr. Jorizzo.
An even smaller portion of people experience symptomatic dermatographism.
Dermatographic urticaria does not seem to have any association with race or ethnicity. Some research suggests that having a family history of the condition increases the risk of developing it. And it appears to be more common in women than men.
Symptoms of dermatographic urticaria
Most people with simple dermatographism develop a line of raised, itchy, red, or flesh-colored skin where the skin has been moderately to firmly rubbed, pressed, scratched, or stroked.
Symptoms tend to develop within one to seven minutes after skin contact, and they reduce or resolve within 30 minutes to an hour.
The symptoms usually correspond to the shape or direction of the skin contact that caused them. For example, scratching the skin may cause vertical lines or streaks, while direct pressure may create a broader, more widespread pattern of impacted skin.
Someone can develop skin writing at any age, though symptoms most commonly begin during young adulthood.
Typically, this condition impacts regions of the skin, though it can impact mucous membranes, such as those that line the mouth and genitals.
In most cases, symptoms of dermatographic urticaria are bothersome and unpleasant but not overly severe or long-lived.
Symptoms of symptomatic dermatographism
People with symptomatic dermatographism develop round hives or lines of round hives and swelling even from very minor, gentle, or light contact.
Symptoms tend to be more severe than with simple dermatographism. They can cause extreme itchiness and burning or prickling sensations. They also tend to last for a few hours or more.
These symptoms also seem to worsen with heat and flare up at night, potentially from the pressure of and contact with bedding.
They may also seem worse at night because the mind is less distracted, giving a person the opportunity to focus more on itchiness, says Anisha B. Patel, MD, associate professor of dermatology at the University of Texas’s McGovern Medical School in Houston.
This type of dermatographism can reduce someone’s quality of life and ability to function, in particular by interfering with sleep and causing stress and anxiety.
How serious is dermatographic urticaria?
In most cases, skin writing is not a serious condition. But people with symptomatic dermatographism may experience painful, stressful symptoms and a reduction in quality of life or the ability to do daily activities.
Typically, there are no complications associated with dermatographism.
However, if you’re taking sedating antihistamines or antianxiety or antidepressant medications, you need to practice caution and make sure you’re not drowsy before driving or operating dangerous machinery.
Open sores caused by dermatographism can also become infected by bacteria or fungus. Left untreated, skin infections can become severe and spread throughout the body.
In rare cases, an extreme, abnormal immune response called sepsis may develop in response to infection. Sepsis causes the immune system to destroy healthy bodily tissues, and it can be fatal.
How is dermatographic urticaria diagnosed?
A dermatologist, a doctor that specializes in the skin, will diagnose dermatographism by stroking the skin and waiting to see if symptoms develop.
“We often take a tool like a tongue depression and with some pressure run it down the skin in a line,” says Dr. Patel. “Within around five minutes or so, if they have dermatographic urticaria, that line where the tongue depressor was applied will become red and raised like a line of hives.”
Skin writing can also be assessed using a dermographometer, a mechanical device that applies varying types of pressure to the skin to see if it causes an excessive reaction.
If you’re being tested for dermatographic urticaria, you’ll want to ease off medications that reduce immune function such as antihistamines; they can lead to false-negative test results.
To get the most accurate diagnosis, avoid antihistamines and other allergy medications for a few days before your appointment.
Talk to a doctor about how to proceed if you’re taking prescription medications that impact the immune system.
How is dermatographic urticaria treated?
The most effective way to treat dermatographism is using antihistamine medications.
Dr. Patel says antihistamines are the main treatment for dermatographic urticaria because symptoms seem to occur due to the overactivity of histamine in the skin.
“Most antihistamines I recommend are over the counter now,” she says. “I often get people to combine different over-the-counter drugs with different mechanisms, such as Benadryl, Zrytec, or Claritin, and Allegra.”
Dr. Patel says someone may need to take high doses of these antihistamines to control their symptoms. But often after a month or so, many people can begin to gradually reduce their dosage.
“The most important thing is to balance side effects of drowsiness from medication with efficacy,” she says. Take a med that makes you sleepy and you could get hurt (or hurt others), depending on the activities you do.
For this reason, nondrowsy antihistamines are usually recommended over sedating antihistamines.
Dr. Jorizzo says he wouldn’t suggest using medications with “D” in the name (think Claritin-D). They typically contain medication that constricts dilated blood vessels in your nose, which isn’t necessary and causes sedation.
If someone does need to take sedating antihistamines, Dr. Patel says it’s best to take them before bedtime or in the evening.
If your dermatographic urticaria is related to another skin condition (such as scabies) or infection, you’ll be treated for that condition as well.
Other treatment options for dermatographism that may help manage symptoms include:
- Anti-anxiety medications
- Antidepressant medications
- Psychological therapy
- Cromolyn, a medication that helps stabilize the skin’s cellular membrane and reduce the release of histamine
Other treatment options still being investigated
Research trials are underway to see test if the medication omalizumab may help treat dermatographic urticaria.
There is also some evidence that light therapy may help treat dermatographism, though most people seem to experience symptoms again two to three months after stopping treatment.
Getting 1,000 milligrams of vitamin C daily may also help reduce symptoms of skin writing by increasing the breakdown and removal of histamine from the body.
Lifestyle tips for living with dermatographic urticaria
By far the most effective way to manage skin writing is to avoid triggers that cause symptoms, especially those that tend to cause the release of histamine.
Not everyone experiences the same set of triggers. But some known causes of dermatographism and hives include:
- Very hot water or steam
- Vigorous or excessive towel rubbing
- Stressful life events or excessive stress or anxiety
- Very cold or warm environments
- Friction from sweating and exercising
- Clothing, undergarments, jewelry, sports equipment, or supportive devices that rub or cause friction
- Antibiotics, especially penicillin
Other lifestyle tips for living with dermatographic urticaria include:
- Wear loose-fitting, comfortable clothes throughout the day and night. Choose breathable fabrics like cotton.
- Wear moisture-wicking clothing.
- Avoid prolonged cold or warm showers, baths, etc.
- Wear fitted clothing while exercising or being physically active to avoid rubbing.
- Use loose, soft, breathable cotton, silk, or satin bedding, which is less likely to cause irritation.
- Reduce itching and dryness with moisturizer.
- Use over-the-counter creams or ointments that prevent itching or numb the skin for 30 to 45 minutes, and apply them as soon as itching develops to prevent scratching and worsening symptoms.
Living with dermatographic urticaria
Many people experience dermatographism flares of symptoms for months to years after they first develop.
On average, idiopathic (of an unknown cause) symptomatic dermatographism can last for six years. But in some cases, dermatographism symptoms may start to reduce within six months after they first developed.
When dermatographism is directly related to a specific trigger, such as a skin disease or specific allergen, symptoms may only last for a few days to weeks.
In many cases, dermatographic urticaria resolves on its own without treatment. But early, effective treatment may reduce the risk of experiencing severe, long-lasting symptoms and complications.


















