Doctors Say Knowing About This Vaccine Could Cut Your Cancer Risk Significantly
Updated: Mar. 08, 2022
The HPV vaccine has become available to more patients in recent years. The bad news? Many patients who could benefit from it have had no idea they're now eligible.
An important change to the HPV vaccine age limit
“I found out I had HPV when I went to the doctor just before I was about to move to Europe for a year,” says a 42-year-old woman who requested to remain anonymous. “I was preparing to go on the adventure of a lifetime, but getting the news terrified me. It was over 15 years ago, I was in my mid-twenties. All I knew about HPV is that it can increase the risk of cervical cancer, and my doctor informed me I had one of the problematic strains.”
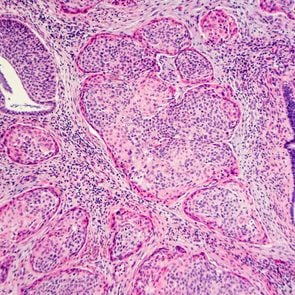
The human papillomavirus (HPV) is a virus that’s transmitted, usually but not always, through sexual activity. The Centers for Disease Control and Prevention (CDC) suggests 13 million Americans become infected with HPV every year.
This is concerning because some strains of the virus has been shown to lead to any of several cancers—it’s best known for being linked with cervical cancer—but also vaginal cancer, vulvar cancer, head and neck cancers, anal cancer, penile cancer, and genital warts. Recent years have brought about the potentially game-changing HPV vaccine that, according to a 2021 BBC report, is slashing cervical cancer rates by a remarkable 90 percent.
The challenge is that many patients who need the HPV vaccine don’t know that it’s now available to them. When HPV vaccine first became available in 2006, it was limited to patients up to 26 years old. In 2018, the U.S. Food & Drug Administration (FDA) approved the HPV vaccine for patients up to age 45—but some patients argue that word didn’t get out. “I go for my annual exam and Pap smear every year, and I still had no idea the vaccine was available to me,” says our anonymous subject. “It was completely by chance I learned about this when I was helping a hospital system with community education about Covid-19 at the start of the pandemic. Otherwise, I still wouldn’t know.”
And, for both males and females, this age limit expansion for the HPV vaccine could be critical. For cervical cancer alone, diagnosis rates dropped approximately 52 percent for women aged 15 to 29 between 1999 and 2017. There’s also mounting evidence that the HPV vaccine may have similar effects on those other HPV-related cancers.
Is the HPV vaccine right for me, or my child?
The HPV shot works best if you haven’t been exposed to HPV—so ideally, before an individual becomes sexually active. This is why early HPV vaccination efforts targeted boys and girls between the ages of 9 and 12.
However, the Advisory Committee on Immunization Practices (ACIP)—a group of medical and public health experts that develops recommendations on how and when to use vaccines—now suggests that some adults aged 27 through 45 years who weren’t already vaccinated could also benefit from the cancer protection offered by these shots.
The original Gardasil covered four HPV strains; while Gardasil9, available since 2014 and now the only HPV vaccine available in the U.S., protects against nine.
Children aged 11 to 12 should receive two doses of HPV vaccine, given 6 to 12 months apart. As it stands, everyone up to age 26 should get HPV vaccine if they were not fully vaccinated already.
Children who start the HPV vaccine series on or after their fifteenth birthday need three doses, given over six months. Three doses of HPV vaccine are also recommended for folks with compromised immune systems.
In some cases, these shots were a tough sell in the beginning, as many parents had safety concerns and were unaware or uncomfortable about the need to protect their children (perhaps specifically boys) from these sexually transmitted diseases and cancers.
Fortunately, times are changing. About 59 percent of U.S. teens were up to date on HPV vaccinations in 2020. This rate has been slowly climbing over the years, according to data from the CDC.
Can I get the HPV shot now?

Some people absolutely can derive protection from the shot later in life, experts say. “It is an extremely safe vaccine and worth getting, even if the benefit isn’t as strong as it was when you were younger,” states Otto Yang, MD, an infectious disease expert at UCLA Health in Los Angeles.
If that’s encouraging, here’s more background: The FDA’s approval of Gardasil9 in women ages 27 to 45 is based on a study of about 3,200 women in this age range. In the three-and-a-half-year longitudinal study, the shots were 88 percent effective at preventing a combined endpoint of persistent HPV infection, genital warts, vulvar and vaginal precancerous lesions, cervical precancerous lesions, and cervical cancer related to HPV types covered by the vaccine. It’s believed to have the same type of efficacy in men in this age range.
The ACIP didn’t recommend catch-up vaccination for all adults aged 27 to 45. Instead, the group stated that some people who have certain risk factors that predispose them to HPV should talk to their doctor about the shots.
This list may include, but is not limited to:
- Men who have sex with men
- Transgender individuals
- People with weakened immune systems
More on whether the HPV vaccine could be right for you
Rhoda Sperling, MD, a professor of obstetrics, gynecology, and reproductive science at the Icahn School of Medicine at Mount Sinai in New York City, suggests the new recommendation for getting vaccinated up to age 45 involves shared clinical decisions or having an open conversation with your doctor. “We talk about Pap tests and other screening tests as well as vaccines, including the HPV shot,” Sperling says of some patients.
Ideally, the HPV vaccine should be administered before potential exposure to HPV through sexual contact, but Sperling explains that the idea is to look at your risks and lifestyle with your doctor. “People who have never been sexually active because they were waiting for marriage or may have new partners after a divorce, or who have a new partner who [had multiple sexual partners] in the past may benefit,” she says.
Kristina Brown, DO, FACOG, an obstetrician-gynecologist in DuBois, PA, agrees. “The annual is the best time to address this,” says Dr. Brown. “If I bring it up, and they say, ‘Tell me more,’ that really opens the conversation for us to weigh the risk and benefits for them and make a decision.”
If a patient is interested in learning more, Dr. Brown first tries to determine whether insurance will cover the costs of the shots. Gardasil9 is covered by most insurance plans for ages 9 to 26 as preventive care, though it’s not always covered for people older than 26, she says.
At what Planned Parenthood reports to be $250 a dose (again, for two to three doses), the cost may be prohibitive—however increasingly, it seems some health coverage providers recognize that a preventive measure such as a shot is better for their bottom lines than more involved treatments for an illness like cancer. “I got my three shots last year, when I was 41,” our subject says. “I was in and out, the nurse administered it every time. Insurance covered the whole thing.”
Other ways to prevent cervical cancer include:
Regular screening tests.
Pap tests can spot pre-cancers early, before they become invasive. Your doctor uses a special tool to gently scrape your cervix to remove cells for testing.
The American College of Obstetricians and Gynecologists recommends that all women undergo cervical cancer screening at age 21, regardless of when you first start having sex. How often you should have cervical cancer screening and which tests you should have will depend on your age and health history, the group states.
Practicing safe sex.
Condoms may provide some protection against HPV, Brown says, though this is not a sure thing.
Not smoking.
Brown adds smoking may also increase your risk for developing cervical and other cancer. (Also read: HPV and Mental Health: OB-GYNs Report How Stress Affects Your Cervical Cancer Risk.)
Sign up for The Healthy newsletter, and continue: