Covid-19 Alert: These Are the Most Promising Vaccines
Updated: Mar. 30, 2022
There are about 200 different Covid-19 vaccines under development, with some showing promise. These four are nearing the finish line.

With the scope of the novel coronavirus (SARS-CoV-2) pandemic worsening by the hour, all eyes are turned to the race to find an effective Covid-19 vaccine. And not just a vaccine, but one that could eventually immunize seven billion people on planet Earth and return us to some semblance of “normal.”
Effective vaccines need to succeed in two ways. “We want to see an immune response that protects the person from that pathogen and we want that immune response to be long-lasting,” says John Cooke, MD, PhD, chair of cardiovascular sciences and medical director of the RNA Therapeutics Research Program at Houston Methodist. Long-lasting, for now, means a minimum of six months. (Find out if it’s possible to get reinfected with coronavirus.)
According to the Milken Institute, 199 vaccines are in various stages of development around the world. A handful of those show promise and are in advanced trials: Someday, hopefully soon, they may be available. (Read more about a family physician’s Covid-19 vaccine trial experience.)
Oxford University
Oxford University seems to be leading the vaccine-development pack with its adenoviral vector vaccine—that’s a mouthful, but here’s what it means: Researchers use a harmless adenovirus (it might cause the sniffles, for example) and imbed it with a piece of the harmful virus (Covid-19, in this case). After the modified adenovirus is injected into your body, your immune system reacts to the harmless invader and knocks it out—and, in the process, learns to recognize the harmful virus. Now, theoretically, you’ll have antibodies that can snuff out the harmful virus should you be exposed.
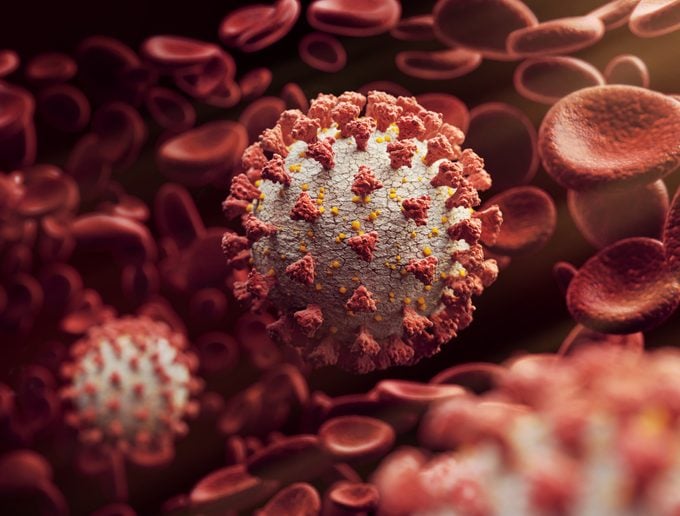 For this particular adenoviral vaccine, U.K. researchers genetically rejiggered a chimp adenovirus (it causes colds) to develop the notorious spike protein found on the surface of SARS-CoV-2. The spike protein essentially punctures the cell wall, allowing the virus to enter and start replicating. Once the adenovirus is injected into people, explains Dr. Cooke, “the immune system [learns to] target that spike protein for attack.” The vaccine is called ChAdOx1, which stands for “Chimpanzee Adenovirus Oxford 1.”
For this particular adenoviral vaccine, U.K. researchers genetically rejiggered a chimp adenovirus (it causes colds) to develop the notorious spike protein found on the surface of SARS-CoV-2. The spike protein essentially punctures the cell wall, allowing the virus to enter and start replicating. Once the adenovirus is injected into people, explains Dr. Cooke, “the immune system [learns to] target that spike protein for attack.” The vaccine is called ChAdOx1, which stands for “Chimpanzee Adenovirus Oxford 1.”
How effective is it?
An early trial among 1,077 healthy people published July 20 in The Lancet found that the vaccine activated the two different parts of the immune system, signaling a good response to Covid-19.
What are the risks?
This would be the world’s first mass-distribution adenoviral vector vaccine for humans, so it’s not yet proven in the real world. Other adenoviral vector vaccines for HIV, influenza, Ebola, and malaria are in trials; the Ebola vaccine was used briefly outside of a trial setting. Even though adenovirus vaccines use a weakened virus, that virus is still active and can cause illness in people with faulty immune systems. (Here’s what doctors want you to know about the AstraZeneca vaccine and blood clots.)
Production and timeline issues
Oxford has signed on with pharmaceutical giant AstraZeneca to produce an initial 400 million doses, with the ability to produce one billion total. AstraZeneca announced that the 400 million doses would be distributed in Europe at no profit to the company and will begin delivering in September. As is the case with most if not all vaccines currently under development, companies are actually making the vaccines as they create them. This is good if the vaccines turn out to be effective but costly for the company if they don’t. “Because of this pandemic, we can’t do things in sequence,” says Dr. Cooke. “Things have to be done in parallel.”
By some estimates, the U.S. Food and Drug Administration may confer emergency-use authorization as soon as October, according to Cornell University. The vaccine is headed for Phase 3 trials which would enroll 10,000 participants in the U.K., 30,000 in the U.S., and 2,000 in Brazil. (All three nations have been hit hard by Covid-19.) Phase 3 is the final phase of testing before a vaccine hits the market, explains Kathryn M. Edwards, MD, professor of pediatrics at Vanderbilt University Medical Center in Nashville.
A second adenovirus vaccine
The Chinese company CanSino Biologics is working on a similar vaccine, Ad5-nCoV, though this one uses a human cold adenovirus married with a gene from the novel coronavirus spike protein. It’s also fairly far along with Phase II trial results published in the same issue of The Lancet showing good safety and immune response. Using a human adenovirus may prove to be problematic, though. “Half of the population already recognizes the common cold virus and [may] destroy it before this vectored vaccine has a chance to work,” he explains.
Moderna
The Moderna mRNA (messenger RNA) vaccine is vying neck and neck with the Oxford vaccine in the sprint to the finish line. This, also, would be the first-of-its-kind in the world. “It’s an entirely new therapeutic approach, which is very exciting,” says Dr. Cooke. This vaccine uses messenger RNA to develop the novel coronavirus spike protein (mRNA carry building instructions for cells, similar to DNA). “You’re just providing the directions where the cell will make a protein,” explains Dr. Cooke.
But rather than adding mRNA to a virus (as is the case with the Oxford vaccine), Moderna scientists have placed it in fatty nanoparticles that, once injected into the body, slide into cells. The spike protein sets off alarm bells, and the immune system learns to recognize and defeat the novel coronavirus—at least, in theory.
How effective is it?
The Moderna vaccine, called mRNA-1273, was the first out of the gate in March when it was tested in 45 human volunteers. Results of that Phase I trial were published June 14 in the New England Journal of Medicine. Like the Oxford vaccine, the Moderna candidate provoked the hoped-for immune response.
What are the risks?
This vaccine would be the first mRNA vaccine, which is a concern for some. “There’s not a single RNA vaccine that’s been approved,” says Dr. Cooke. “That being said, all of the animal work that’s been done and now early clinical trials suggest it can work.” The vaccine also caused side effects. More than half the volunteers experienced fatigue, chills, headache, muscle aches as well as pain at the injection site. The vaccine required two doses and side effects were more evident after the second.
Production and timeline issues
“RNA vaccines can be manufactured very rapidly,” says Dr. Cooke. “Moderna had made their vaccine and got it into clinical trials 42 days after the genetic code of SARS-CoV-2 was published in January.” In late July, the company started its Phase 3 trials. “They’ll have a placebo then a vaccine, participants will be followed for side effects and to see if they make antibodies,” says Dr. Edwards. “The real question is do any of them get Covid-19.” Any participants who show Covid-19 symptoms will be tested for SARS-CoV-2 and all participants will be told to take precautions to prevent getting infected, she adds. Moderna says it will be able to produce and deliver about 500 million doses a year, possibly as many as one billion, starting in 2021.
Sinovac
Vaccine developers are also relying on more traditional methods of making vaccines. “This would be to give a weakened form of the pathogen,” explains Dr. Cooke. Similar to the adenovirus vaccines under development, this stimulates the immune system to produce antibodies to attach the virus. Sometimes the vaccines use killed viruses. A Chinese company, Sinovac, is using this approach in its experimental product, CoronaVac, and seems to be the lead, according to Cornell University. (Here are the vaccine myths you can safely ignore.)
How effective is it?
A company statement issued June 13 said simply that 90 percent of participants in a Phase 1/2 trial had antibodies responses and that the vaccine had no significant side effects. The vaccine had previously been effective in rodents and non-human primates, according to a paper published previously in Science.
What are the risks?
Like adenovirus vaccines, vaccines using weakened virus particles can sicken vulnerable individuals.
Production and timeline issues
Traditional vaccines using attenuated viruses take forever to make so this vaccine, even if proven effective likely wouldn’t be the first on the market.
Inovio
Not unlike the mRNA vaccine, Inovio’s DNA vaccine involves giving your cells instructions to produce SARS-CoV-2 proteins. With the right directions, the cells can then produce their own proteins which then spur an immune response. Instead of using mRNA, though, the vaccine uses actual DNA. This is also an entirely new technology, though Inovio has worked on a similar vaccine for Middle East Respiratory Syndrome (MERS), another coronavirus which erupted in Saudi Arabia in 2012.
How effective is it?
At the end of June, the company reported that 94 percent (34 out of 36) volunteers in a Phase 1 trial produced immune responses to the vaccine, called INO-4800. The vaccine also appeared to be safe with minimal side effects. It’s not clear if the data has been peer-reviewed.
What are the risks?
This technology is unproven and, like Moderna, Inovio has never developed an approved product, says Cornell University.
Production and timeline issues
Inovio said it plans to begin Phase 2/3 trials this summer. DNA vaccines (there are several others in development) are fairly quick to turn around, says Dr. Cooke.
When will we see a vaccine?
All of the candidate vaccines face the same production issues: being able to manufacture enough vaccine for the whole world. Existing manufacturing plans are much smaller than needed to produce vaccines for a pandemic. That means entirely new facilities are being built from scratch. Some, namely Moderna and Oxford University, are further ahead than others on several fronts.
“The studies are going to have about six months of follow-up so I think that would put the efficacy data available probably at the earliest at the end of the year,” says Dr. Edwards. Then there’s the approval process, although she anticipates the FDA will do that right away if the results are clear. (Next, learn about the vaccinations you need but aren’t getting.)















