HPV and Mental Health: OB-GYNs Report How Stress Affects Your Cervical Cancer Risk
Updated: Jul. 06, 2022
These doctors specializing in women's health—including a gynecological cancer doctor—say that when you take care of your mind, you're taking better care of your body, too.
What is HPV?
HPV stands for the human papillomavirus: A virus that is most commonly, though not always, transmitted through sexual contact. Whether you’re male or female, if you’ve ever received an HPV diagnosis, it can feel isolating and scary… but you’re definitely not alone.
In fact globally, HPV is the most common sexually transmitted infection, according to Hoosna Haque, MD, a specialist in obstetrics and gynecology and faculty member at Columbia University Irving Medical Center. “It’s estimated that 80 percent of people who are sexually active will have at least one type of HPV at some point in their lifetime,” Haque explains. The Centers for Disease Control and Prevention (CDC) reports that percentage translates to 13 million new HPV infections each year in the U.S. alone. (Read why doctors say you should stay encouraged even after being diagnosed with HPV.)
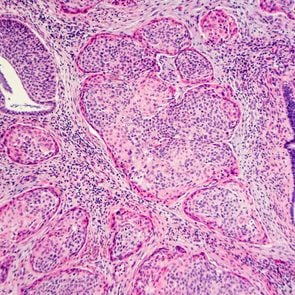
The World Health Organization suggests that nine times out of 10, an HPV infection doesn’t lead to serious problems. However, Dr. Haque cautions, it’s that 10 percent of persistent infections with high-risk strains of the virus that concern doctors. Dr. Haque says that over the course of 10 to 20 years, or even longer, these HPV strains can lead to various types of cancer. Cervical cancer in specific is so significantly linked with HPV that the standard recommendation for yearly Pap smears in the U.S. has led to a 50 percent drop in the rate of cervical cancer diagnoses since the 1970s.
How HPV can lead to cervical cancer
Aside from being diagnosed with one of the high-risk strains, Dr. Haque says there’s not a surefire way to know exactly who will develop cancer or other health problems from HPV. That said, research shows certain factors can make it more challenging for your body to clear infections, like HPV.
For example, any condition that suppresses or weakens the immune system can make it harder for someone to fight off this virus. This could include HIV, lupus, a form of cancer, or another health issue, says Dr. Cheruba Prabakar, a board-certified obstetrician and gynecologist.
Lifestyle choices matter, too. Dr. Prabakar explains the importance of keeping your immune system in great shape by eating a balanced diet, exercising, and getting enough sleep. And, interestingly, “[…S]topping smoking helps clear HPV much faster,” she says. Further, a study in the European Journal of Cancer identified cigarette smoking as an independent risk factor for cervical cancer—and that the risk of HPV developing into cervical cancer decreases when you drop the habit. (Explore our 22 best ways for how to quit smoking.)
Another potential culprit for the presence and persistence of HPV in women? A 2021 Swiss psychotherapy study published in the peer-reviewed BMC Cancer suggests chronic stress may play a role in HPV-related cancers.
What is chronic stress?
We all know isolated high-stress events are inevitable throughout life, whether you face sudden unemployment, a breakup, a major work deadline, a loved one’s death, or something else. In these cases, your body’s built-in stress response can actually be beneficial to your health. “Stress is needed in our lives to release adrenaline and give us that pick-me-up, kick-in-the-butt to help us forge ahead, embark on and complete goals and projects, and even improve performance,” says Dr. Sanam Hafeez, a neuropsychologist in New York City and director of Comprehend the Mind.
But on the other hand, an accumulation of persistent, daily stress takes a toll on your health, explains Janine Ilsley, LMSW, an integrative therapist at Cobb Psychotherapy in New York. Ilsley says modern-day stress takes the same toll as it did on our ancestors, even though they faced a different set of challenges, fears, and frustrations.
Here’s a pared-down explanation of how stress affects your brain: The rational frontal cortex can tell the difference between a physical threat and an emotional one. The amygdala—the emotional side of your brain that triggers the fight, flight, or freeze response—does not.
In other words, when you experience an ongoing cycle of worry or trauma, your primal threat-detecting sensors can get stuck on overdrive. As a result, it’s possible to become caught in a cycle of chronic stress.
How is chronic stress related to HPV?
Dr. Hafeez says that once the stress response is set off, your body produces the hormone known as cortisol. Cortisol works to manage blood sugar levels, supplying the appropriate energy your body requires to deal with the stress at hand until that threat passes.
As this happens, cortisol also suppresses other physiological processes (including reproductive, digestive, and immune functions) that are more or less unnecessary in the fight-or-flight scenario. For our ancestors running from a mountain lion, these functions would return to normal once they’d reached safety and cortisol levels dropped. But in today’s world where it might feel like worry is inescapable, many people live with constant stressors present.
To that end, cortisol production stays activated and continues to suppress the body’s normal processes… including your immunity. That’s why research links chronic stress with a huge range of health conditions, such as mental health disorders, heart disease, diabetes, and infectious diseases.
And, yes: The 2021 Swiss study found that stress is an independent risk factor for HPV presence and persistence in young women, as the research team stated their findings suggest that “chronic stress and diurnal cortisol are related to the presence of [HPV] infection and may thus play a role in HPV-associated cervical carcinogenesis.” (Carcinogenesis is defined as the start of cancer formation.)
Based on the researchers’ conclusion, chronic stress may play a role in the potential that HPV infection will remain active and eventually turn cancerous.
Ways to lessen your HPV risk

The persistence of an HPV infection remains the greatest risk factor in the virus’s potential for turning into cancer. That’s why keeping your immune system in fighting form is one of your best defenses against HPV.
How to strengthen your immune system
“The more healthy—physically and mentally—a patient can be, the better their chance of fighting and clearing the virus,” says Jessica Lee, MD, OB-GYN at the University of Maryland Medical Center and Assistant Professor at the University of Maryland School of Medicine in Baltimore. This includes getting enough exercise, getting enough sleep, and eating a nutrient-rich diet—all things that promote a high-functioning immune system.
John Diaz, MD, chief of Gynecologic Oncology and lead physician for clinical trials in Gynecologic Oncology at Miami Cancer Institute says that “limiting those things that are hampering our immune system” is important to staying well. “Make sure your alcohol intake is moderate, don’t smoke, all those things that we all know we should do better at really make a difference on how well the immune system can clear that HPV infection,” he advises.
Practice safe sex
“I always tell patients that if you have unprotected sex with somebody, you are getting every type of HPV that person has—and that of everybody they’ve ever slept with,” Dr. Prabakar says.
She explains that if someone gets reinfected with HPV, it doesn’t give their body a chance to really clear a strain before contracting another one. “And if your body doesn’t clear it, it can slowly, over time, cause cervical changes that can eventually lead to cervical cancer,” she says.
Get vaccinated
“The HPV vaccine protects against the most common and most aggressive cancer-causing strains of HPV and the strains that cause genital warts,” Dr. Haque says.
The HPV vaccine works extremely well. A November 2021 study published in The Lancet found that since the vaccine’s introduction in the United Kingdom in 2008, cervical cancer cases fell by as much as 87 percent.
Other studies have found that this protection is long-lasting, too. According to the Centers for Disease Control and Prevention, researchers have found no evidence that the vaccine’s effectiveness decreases over time.
Also, it’s important to note that the HPV vaccine is not just for women. “We’ve learned a lot more about the potential impact of HPV on men, including [head and neck] cancer, anal cancers, and rarely, penile cancer,” Dr. Diaz says. “So this vaccine helps protect them against all that.”
In the U.S., the CDC recommends boys and girls receive the HPV vaccination around the ages of 11 or 12 (though it’s approved from age 9 to age 45.)
“Unvaccinated adults should discuss the benefits of vaccination with their doctors, as although they will likely have been exposed to HPV, there will still be benefits to immunization,” Dr. Haque says.
Interested in getting the HPV vaccine as an adult? Here’s what you should know.
Get regular screenings
Between HPV vaccinations and routine cervical cancer screening, we really should be able to eliminate this disease in the U.S., says Dr. Diaz. “Unfortunately, what we’ve seen over the last couple of years is that because of the pandemic, many women were not able to undergo their recommended screening,” he says.
In fact, a study published in Morbidity and Mortality Weekly Report shows that in California, HPV screening rates dropped 82 percent during 2020. “And so we’ve seen a little bit of a bump in new cervical cancer cases,” Dr. Diaz explains, possibly due to the lack of screening and followup during the Covid-19 pandemic. “Women really need to make sure that they’re seeing their gynecologist every year,” he says. Read more on this in How Often Should You Get a Pap Smear?
Manage stress to manage HPV and fight cervical cancer
As the 2021 Swiss psychotherapy research shows, managing your stress levels is crucial for a healthy immune response. Diet, exercise, rest, meditation, getting fresh air, and making time for hobbies each contribute to better stress management.
But, Dr. Hafeez says: if you still feel like your stress is unmanageable, seek out therapy from a mental health professional to help build coping mechanisms that work for you.
For more self-care and wellness wisdom, sign up for The Healthy‘s daily newsletter. Then, continue:
10 Easy Self-Care Swaps to Make in 2022
Create the Ultimate Meditation Space: Mindfulness Experts Share 4 Easy Ideas
Is Walking Good Exercise? Fitness Pros Explain Why It’s an Ideal Workout
The Banana Health Benefit You for Sure Weren’t Aware Of, Dietitians Reveal