How to Keep Your Feet Healthy if You Have Diabetes
Updated: Apr. 29, 2021
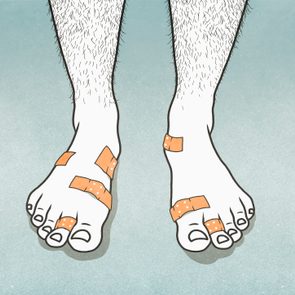
Foot care is an important part of managing diabetes. Follow this diabetes foot care guide to find out how to identify problems early, get blisters and sores treated, and avoid diabetes-related foot problems in general.
On This Page
What is diabetes foot care?
If you have diabetes, you know management is about more than just maintaining a healthy diet and controlling your blood sugar. Diabetes can affect every system and part of the body.
One area that requires a significant amount of attention is your feet. “The raising of blood sugar can damage the nerves and thereby affect the sensation in the feet, causing foot problems to arise,” explains podiatric surgeon Rebecca Pruthi, DPM, owner of Foot Care of Manhattan in New York City.
Therefore, it’s important to practice proper diabetic foot care to help prevent foot problems from happening.
Causes of diabetic foot problems
“Foot problems are very common in people with diabetes as multiple systems, especially the neurological and circulatory, are impacted,” says podiatrist and wound specialist Desmond Bell, DPM, the founder and president of the Save a Leg, Save a Life Foundation in Ponte Vedra, Florida. “And the feet are the area that is often where symptoms first appear.”
Damage to these systems, which causes a loss of sensation and decreased blood flow in the legs and feet, is the primary instigator for the development of foot problems in people with diabetes. In addition, the damage causes these problems to heal more slowly and worsen more rapidly.
On the neurological side, up to 50 percent of people with diabetes experience peripheral neuropathy. “Neuropathy is a condition in which nerve damage occurs because blood glucose levels are too high,” says Dr. Pruthi. “It is thought that uncontrolled high blood sugar damages the nerves by interfering with their ability to send signals.”
And on the circulatory side, roughly one-third of people with diabetes have to deal with peripheral arterial disease, or PAD.
“Elevated blood glucose causes chronic inflammation within the arteries of the body, which leads to plaque formation and decreased blood flow due to narrowing or blockage of the vessels,” explains Dr. Bell. “When this occurs outside of the heart vessels, and especially in the lower extremities, it is referred to as peripheral arterial disease.
This damages both the larger arteries that supply blood to the structures within the legs and feet and the smaller blood vessels that supply the skin.” The result: An increased risk for surface wounds, infections, amputation, and even death.

Symptoms of diabetic foot problems
The symptoms of neuropathy and PAD are typically the first indicators that diabetes is affecting your foot health. According to our experts, these may include any of the following, experienced in one or both feet:
- Numbness or an inability to feel pain or temperature
- Tingling or burning
- Sharp pains or cramps
- Increased sensitivity to touch
- A feeling of “fullness” in the feet (this can occur in the hands as well)
If these symptoms are ignored or left unchecked, they can lead to or worsen foot problems down the road. Some of these include:
- Skin issues, such as athlete’s foot, fungal nails, dry skin, and calluses
- Diabetic blisters
- Foot ulcers
- Infections
- Gangrene
- Structural deformities, such as hammertoes, claw toes, and mallet toes
- Spontaneous fractures, also known as “Charcot’s foot,” which can cause collapsed arches and the formation of pressure points on the foot in places they aren’t meant to be
Preventing diabetic foot problems
“We want patients to become proactive versus reactive when it comes to addressing these issues,” says Dr. Bell. Fortunately, there are many steps you can take to protect your feet from the problems associated with diabetes.
Maintain a healthy diet and blood sugar. The more regular your blood sugar is, the less likely you are to develop foot issues. (Here are foods that may help improve your circulation.)
Choose the right shoes. “Wearing cushioned, supportive shoes is key to avoid pinching, calluses and ulcers from forming,” says Dr. Pruthi. (Here are tips on choosing the right diabetic shoes for you.) Dr. Bell recommends getting your foot measured by a professional to make sure you’re wearing the right size. Also smart: Always check shoes for pebbles or other debris before slipping them on.
Avoid going barefoot. Explains Dr. Bell: “Stepping on objects, either sharp or dull, or on a hot surface can create trauma that may result in wounds, infection, or amputation.” (Learn more why walking barefoot is bad for your feet.)
Inspect your feet at least twice daily. “You want to look for any changes, including blisters, open sores, excessive moisture between the toes, or any signs of infection,” says Dr. Bell. “Also, beware of toes or feet that appear with increasing redness, blanching, or bluish discoloration. These can be signs of decreased blood flow.” If you don’t have the flexibility to examine your feet closely, use a handheld mirror placed on the ground to inspect the soles of your feet.
Wash your feet daily. Keeping your feet clean is an integral part of preventing infections. But this should be an active process, never just a soaking. “Those who have lost protective sensation in their feet are at risk for scalding if the water is too hot,” Dr. Bell says. “Also, extensive soaking can lead to excessive drying of the skin, which opens up undetectable cracks in the skin that can be a portal of entry for bacteria, fungus, or viruses.” To prevent dryness, moisturizing regularly is also key.
Don’t cut your own toenails. That’s a job for a podiatrist, says Dr. Pruthi. Mishandled clippers can cause injuries or create tiny cuts through which bacteria can enter and allow infections to flourish.
Exercise. “Exercise is always recommended, especially when supervised,” says Dr. Bell. “Walking is a great way to begin an exercise program, provided that you have proper-fitting shoes and/or protective insoles.”
Treating diabetic foot problems
If you notice something wrong with your feet, act fast. “Waiting for things to get better usually results in the opposite occurring,” says Dr. Bell. If you see a podiatrist, he or she can help you take the proper steps to heal—and if those steps are taken promptly, most people with diabetes are able to avoid serious consequences like an amputation. Depending on the nature of your injury or problem, steps may include:
Keeping the injury clean and dry. Even if you only get a small cut on your foot, diabetes slows down the healing process, increasing your risk of infection. To avoid infection, keeping the injury clean, dry, and protected is key. That means cleaning it daily per your doctor’s advice and keeping it covered with a clean bandage and dressing.
Staying off of it. Whether you have a spontaneous fracture or a foot ulcer, removing any pressure from the area will help speed up healing. That could involve wearing special shoes or orthotics that reduce pressure on a particular part of the foot, using a brace, or walking with crutches.
Antibiotics and debridement. Two additional steps can reduce your risk of infection. Antibiotics are prescribed to fight any present infection and debridement involves removing any calluses, infected or dead tissue, and foreign debris from the wound. This should be under the guidance of a well-trained podiatrist or wound physician.
Assisted wound closure. For foot ulcers that won’t heal on their own, a procedure called vacuum-assisted wound closure can be used. This procedure uses a device that decreases air pressure around the wound, which helps reduce swelling and pull the edges of the ulcer together.
Angioplasty and stents. If you have poor circulation or peripheral arterial disease, you will need revascularization for the wound to heal. This means procedures like angioplasty and placing stents to open the arteries in the legs and restore blood flow to the feet, preventing gangrene, limb death, and possibly amputation.
Personal stories
Stories of people who have experienced diabetes-related foot problems can help you cope with your own. Here are some that show what it’s like to live with this issue.
- This Woman with Diabetes Almost Lost Her Leg Due to an Ant Bite
- This Doctor Is Saving Limbs in Black Patients with Diabetes
Helpful products for diabetic foot care
Proper foot care starts with choosing the right shoe for your needs. Shoes can make a big difference when it comes to preventing diabetic foot problems. Here are some podiatrist-recommended products that may help provide you with some much-needed comfort and support whether it’s for walking, work, home, travel, or exercise.
- The 10 Best Diabetic Shoes for Women
- The 10 Best Diabetic Shoes for Men
- The 10 Best Shoes for Neuropathy
- The 10 Best Diabetic Slippers for Men
- The 10 Best Diabetic Sandals for Women
Additional resources
If you would like to learn more about diabetic foot care, here are some additional resources: