
What to know about birth control methods
The 1960 invention of the first birth control method—the pill—fundamentally changed sex and our lives ever since. While contraception methods have been around since prehistoric times (think: animal intestine condoms…for real!) the existence of safe, reliable ways for women to plan and control childbearing has had radical societal effects. For one, a 2020 report from the United States Congressional Joint Economic Committee suggested that contraceptive access is linked with today’s rates of women in higher education and representation across the workforce. The Institute for Women’s Policy Research has also noted that birth control access may even predict greater earning potential for females.
In the decades since the pill’s commercial launch, a variety of birth control methods have come available to suit women’s varied physiologies, lifestyles and preferences. And today, nearly all sexually active American women report having used some form of birth control, according to the American College of Obstetricians and Gynecologists.

What’s the best birth control method?
With today’s birth control options, women have more control over how they want to manage contraception. Jennifer Roelands, MD, OB/GYN, and owner of Well Woman MD, says she asks her patients two key questions as they weigh what’s best for them:
-
Is it important for you to have a period every month?
-
Will you remember to take or use your contraception?
“If you have some medical conditions, certain birth control may not be recommended,” adds Monte Swarup, MD, FACOG, OB/GYN, and founder of Vaginal Health Hub. Dr. Swarup adds that if you have multiple partners, it’s important to consider options that will protect you against sexually transmitted diseases (STDs).
All in all, there’s no one-size-fits-all solution, and it can take women a bit of trial-and-error to find the right option—or combo—to suit her needs.
How’s Your Sexual Hygiene? A Doctor Says This Habit Is a Must (for Singles, Too)

The pill
“Even today, the traditional birth control pill is still the most popular form of contraception,” says Susan Lipinski, MD, OB/GYN at Obstetrix of Colorado, part of Pediatrix Medical Group. All pills work by dabbling with your hormone levels—specifically progesterone and/or estrogen—to suppress ovulation and thin your uterine lining. “There are many different combinations of estrogen and progesterone at different doses, but all are of similar efficacy,” Dr. Lipinksi says.
When it’s taken every day at the same time, effectiveness can be as high as 99% (though in practice, this is closer to 91%, according to Dr. Swarup). The pill tends to make periods lighter, more regular and less painful—and it can be used to treat other conditions, like ovarian cysts, endometriosis, pre-menstrual dysmorphic disorder (PMDD) and acne.
The pill also gives you a lot of control over your period, even skipping it altogether. Seasonale was the first brand to market this advantage, designing its pill packs so that you only have a placebo week (and bleed) every three cycles. “You can do that with most birth control pills, just skip the placebo week and go to the next pack,” Dr. Roelands says.
As for the cons of the pill: you have to remember to take it every day, it can increase the risk of blood clots for certain women and they don’t protect against STDs. “Some women are very sensitive to hormones and changes in hormones,” Dr. Lipinski says, adding that for some, “[the pill] can trigger depression symptoms.”
Healing My Gut with Probiotics Relieved My Depression: I Tried It

Other hormonal methods
Most hormonal birth control methods share similar benefits (and disadvantages) with the pill—but each has its own additional considerations that could make it an ideal option for some women, while a no-go for others.
Vanessa Lachey Gets Candid about Her Longtime Health Struggle—and the #1 Key to Her Marriage

The vaginal ring
“The benefit of these is that the user controls inserting and removing the ring,” Dr. Lipinski says—and once it’s in, you don’t have to remember to take it daily.
The Nuvaring was first released in 2001 and designed to be replaced monthly. “Annovera is the newest option on the market,” Dr. Lipinski says. It’s left in place continuously for 21 days, taken out for a week, and then replaced again, reused monthly for one year. On average, the ring as a form of birth control is reportedly 91% effective.
11 Important Things Your Vaginal Discharge Can Reveal About Your Health

The patch
The Ortho Evra patch contains estrogen and progestin (like the combination pill), but you change it weekly instead of taking it daily, Dr. Lipinski says. “It has the same risks as [the pill and the ring].” It’s also about 91% effective.
While it’s not yet commercially available, researchers are also currently developing a painless microneedle patch that works like this: the patch is pressed into the skin for three seconds and left in place for about a minute longer. During this application, microneedles embed in the skin to slowly release a contraceptive hormone over the course of a month.
Doctors Say Knowing About This Vaccine Could Cut Your Cancer Risk Significantly

The injection
As there’s almost no room for human error, the contraceptive injection (the most common being Depo-Provera) is among the most effective forms of birth control. It’s also long-acting—you only have to get it administered every 12 weeks (but it has to be at your doctor’s office) and can expect about 94% effectiveness throughout.
The shot does not contain estrogen, either, so it’s a safer hormone-based option for women at risk of blood clots (like if you are over 35 and smoke, have a history of heart disease, or get migraines). “A downside is that some women do not start ovulating again for up to one year after stopping use,” Dr. Lipinski says. “This means that it can take a long time to get pregnant when you go off the shot.”
Depo-Provera is the only form of birth control studies show can cause weight gain, too. “It works at the brain level to suppress you from cycling,” Dr. Roelands explains. “And so by doing that, it can actually disrupt the messages of whether or not you think you’re full—so people can eat more on Depo.”
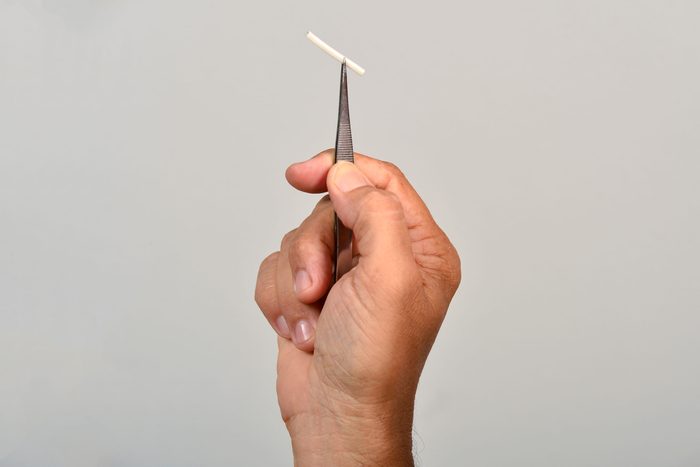
The implant
“[Nexplanon] is an arm implant that can stay in place for continous birth control for up to three years,” Dr. Lipinski says. “It is very effective (about 99%) and does not contain estrogen, so the risk of blood clot or stroke is very low.”
Nexplanon also easy to remove—and you can get pregnant as soon as the next month. “The biggest downside is irregular bleeding,” she adds. “Many women have no bleeding with the Nexplanon, but some have frequent and irregular bleeding.”

The hormonal IUD
“There are multiple different progesterone-releasing IUDs on the market that are good for three to five years, depending on the device,” Dr. Lipinski says. Hormonal IUDs are known to make periods lighter and less painful, and she says that they’re sometimes used to treat heavy periods or endometriosis. “Since the hormone is working just in the uterus, they do not increase the risk of blood clots or stroke,” she says. IUDs are also known to have a 99% efficacy rate or higher, and then “after removal, you can become pregnant as soon as the next month.”
Can a Menstrual Cup Displace an IUD? A Doctor Says It’s a “Growing” Problem

Non-hormonal birth control methods
Most barrier birth control methods have lower efficacy rates than their hormonal counterparts. That’s largely because you have to remember to use them—and use them correctly—every time you have sex. This includes condoms (82% effective) and diaphragms (88%), the female condom (79%), the cervical cap (77 to 83%), the sponge (76 to 88%) and spermicide (72%).
“There is a new non-hormonal vaginal gel called Phexxi,” Dr. Swarup adds. Phexxi is said to be about 86% effective—more effective than spermicide—and alters the vaginal pH to make it inhospitable to sperm. “In many cases, women use Phexxi in combination with other forms of birth control such as the pill or condoms, and when combined it’s even more effective,” Dr. Swarup says.
“The rhythm method” is another birth control method that relies on tracking your menstrual cycle to identify which days you’re least fertile. This fertility awareness method is about 76% effective at preventing pregnancy, Dr. Swarup says, but it requires training and periodic abstinence.
If you’re looking for the most effective form of birth control without hormones, the copper IUD may be the way to go. (The best-known brand on the market is Paragard, whose representatives note that Paragard has been FDA-approved for more than 30 years.)
The copper IUD is reportedly at least 99% effective at preventing pregnancy, Dr. Swarup says, and can last up to 10 years. According to Dr. Lipinski, the biggest downside to keep in mind is that some women experience heavier periods after their copper IUD is placed.
Thinking about getting an IUD? Here are 6 signs it’ll be a good switch for you
For more wellness updates, follow The Healthy on Facebook, Instagram, and Twitter. Keep reading:

